AUCTORES
Globalize your Research
Case Report | DOI: https://doi.org/10.31579/IJBR-2022/066
¹ Emergency Department, Fedail Hospital, Khartoum, Sudan.
2 General Medicine Department, Fedail Hospital, Khartoum, Sudan.
3 Fedail hospital, Khartoum, Sudan
*Corresponding Author: Sarra Hussein Mohamed, Emergency Department, Fedail Hospital, Khartoum, Sudan
Citation: Sarra H. Mohamed, Ashraf M. Osman Ismail, Hussam A. Ali. (2022). Sporadic Creutzfeldt-Jakob Disease Linked to A Possible Dietary Risk Factor, A Case Report. International J. of Biomed Research. 2(6): DOI: 10.31579/IJBR-2022/066
Copyright: © 2022 Sarra Hussein Mohamed, This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 02 February 2022 | Accepted: 25 February 2022 | Published: 16 May 2022
Keywords: sporadic CJD; prion diseases; clinical picture; diagnostic method; dietary consumption
Creutzfeldt-Jackob disease is one of the prion diseases that exhibits lethal neurological consequences and has three distinctive forms: sporadic, genetic, and acquired. The disease is characterized by rapidly progressive multifocal dementia and myoclonus and eventually death within few months. Several diagnostic modalities proved to have high diagnostic accuracy and spared the need for brain biopsy. We describe an old lady who died after forty days of a diagnosis of sporadic Creutzfeldt-Jakob disease based on her presentation of a progressive multifocal dementia, periodic triphasic waves on electroencephalography, and scattered hyperintensities in magnetic resonance imaging. We assumed her diet was the triggering factor for her disease. Given the scarcity of evidence on dietary factors as a trigger factor for sporadic CJD, we would like to report this case.
Creutzfeldt-Jakob disease (CJD) is the commonest among prion diseases that causes irreversible degenerative neurologic condition due to accumulation of pathologic infectious form prion scrapie (PrPsc) in the brain leading to neuronal loss and induce the classic spongiform change (vacuolation of gray matter) [1,2]. The disease is characterized by rapid progressive multifocal dementia with myoclonus, in addition to heterogenous neurological symptoms [1–3]. It has an approximate annual incidence of 1.0 to 1.5 per million globally and the onset of the disease varies between 12-96 years of age [1,2]. Risk factors for developing the disease depend on the classification of CJD to sporadic, genetic and acquired [1–3]. The commonest form is sporadic CJD (sCJD) and is thought to result from a consequence of a rare stochastic event, or somatic mutation of the PrP gene [3]. There is scarcity of evidence on environmental risk factors [3]. Definitive diagnosis is by brain biopsy, but the sensitivity is low, nevertheless, less invasive diagnostic approach yields to have high diagnostic accuracy. Unfortunately, there is no curative medication and the mortality rate is 100% [1–3].
The history was obtained from the patient’s relatives. An 83-year-old lady presented with a rapid deterioration in her neurological status and died within forty days from the initial presentation.
Her initial symptoms started with low grade fever, cough, tiredness, and poor sleep. At the same time, she suffered from auditory hallucination leading her to be agitated and aggressive. These symptoms were followed by deterioration of her recent and remote memory, lack of concentration and person orientation, interrupted speech with word repetition and left gaze fixation, as well as abnormal repeated jerky movement in her right arm. Her walking was affected by short shuffling gait. Her daily living activities had been severely affected such as drinking, eating, and dressing. During her last days, she developed akinetic mutism as she became very calm and speechless. Her sphincters remained intact.
Her systematic review was unremarkable. Her cognitive function was fully intact. She had a well-controlled hypertension, gout, and fatty liver disease. She had neither had surgery before nor did she have blood transfusion, organ transplantation or hormonal therapy. There was no family history of dementia or any neurological diseases of similar condition. Her dietary history revealed significant consumption of meat product. From her youth up to 2002, she consumed meat as a main dish on a daily base and the consumption could reach up to twice per day. The meet will be well cooked but occasionally she would eat a raw liver. She had a preference to sheep’s head and tongue, besides, she used to eat a meal with intestinal content with every sheep that had been slayed. After the diagnosis of gout in 2003, her meat consumption had declined to 2-3 times per week. A further reduction in meat consumption was made in 2014 where she was diagnosed with fatty liver.
The clinical assessment demonstrated a confused, apathetic, and very sleepy lady. Her neurological examination revealed a Glasgow coma scale 12/15, reactive pupils with a left fixed gaze, scattered myoclonus jerk over her body. The tone in all limbs was normal, the power of the motor function was given a score of four. The dementia test was difficult to be assessed due to her confusion. Also, the higher function, cranial nerves and cerebellar function were not easy to be assessed. Her other systems remained intact with no abnormalities detected.
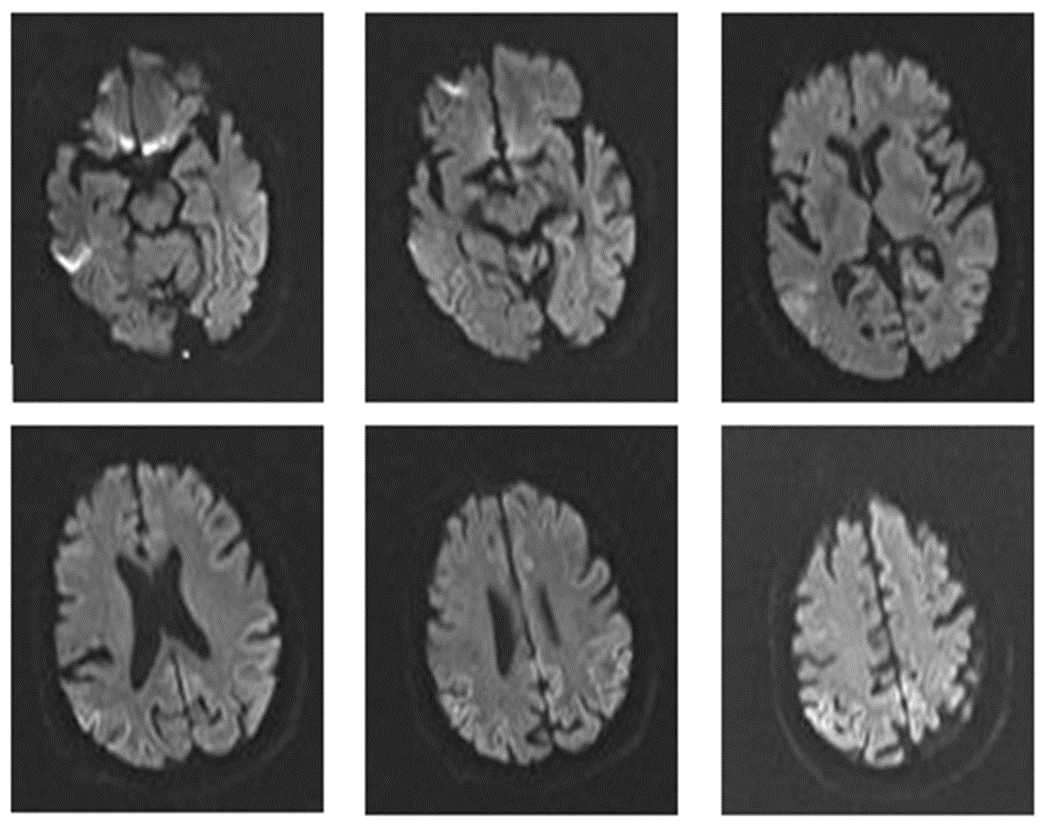
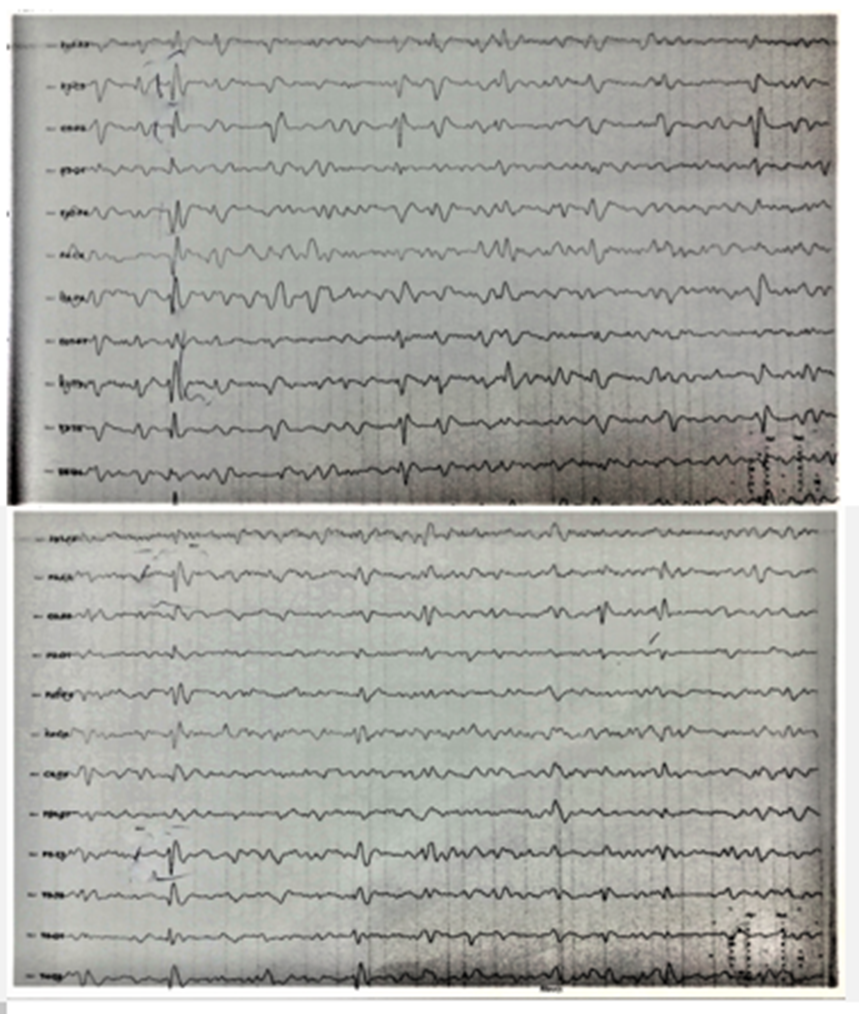
Her routine laboratory blood tests, complete blood count, renal function test, liver function test, thyroid function, and vitamin B12 and Folate were normal. An abdominal ultrasound was consistent with fatty liver disease. Brain imagines were done to exclude any serious neurological event. Initially, a computerized scan (CT) for brain reports no abnormality which is followed by magnetic resonance imaging (MRI) (figure1). On diffusion weight imaging (DWI), asymmetrical hyperintensities involving mainly the parieto-occipital cortex, cingulate gyrus, and left neocortex were noticed. The changes on DWI were more visible than in fluid-attenuated inversion recovery (FLAIR). Apparent diffusion coefficient (ADC) showed cortical low signal. Electroencephalography (EEG) illustrated periodic triphasic waves complexes (figure 2). Cerebrospinal fluid (CSF) analysis reported high protein content 62.2mg/dl but normal cells and sugar.
Given the above-mentioned clinical picture, EEG findings and the features in the MRI we diagnosed her a case of sporadic CJD a form of progressive dementia. The patient was put on supportive treatment to control her symptoms and was discharged with an appointment of an MRI brain to follow the decreased intensities that develop latter in advance disease. Sadly, we had been notified by her son that she rapidly deteriorated and died.
In 1922, Speilmeyer gave the name of this disorder as Creutzfelt-Jakob disease, after he reviewed six cases reported by Creutzfelt in 1920 and Jakob in 1921, and only two matched the diagnostic criteria for CJD (2–4).
The diagnosis of rapid progressive dementia requires combination of clinical picture and certain investigations to guide toward the diagnosis. In this lady, the clinical presentation was typical of that described in CJD.
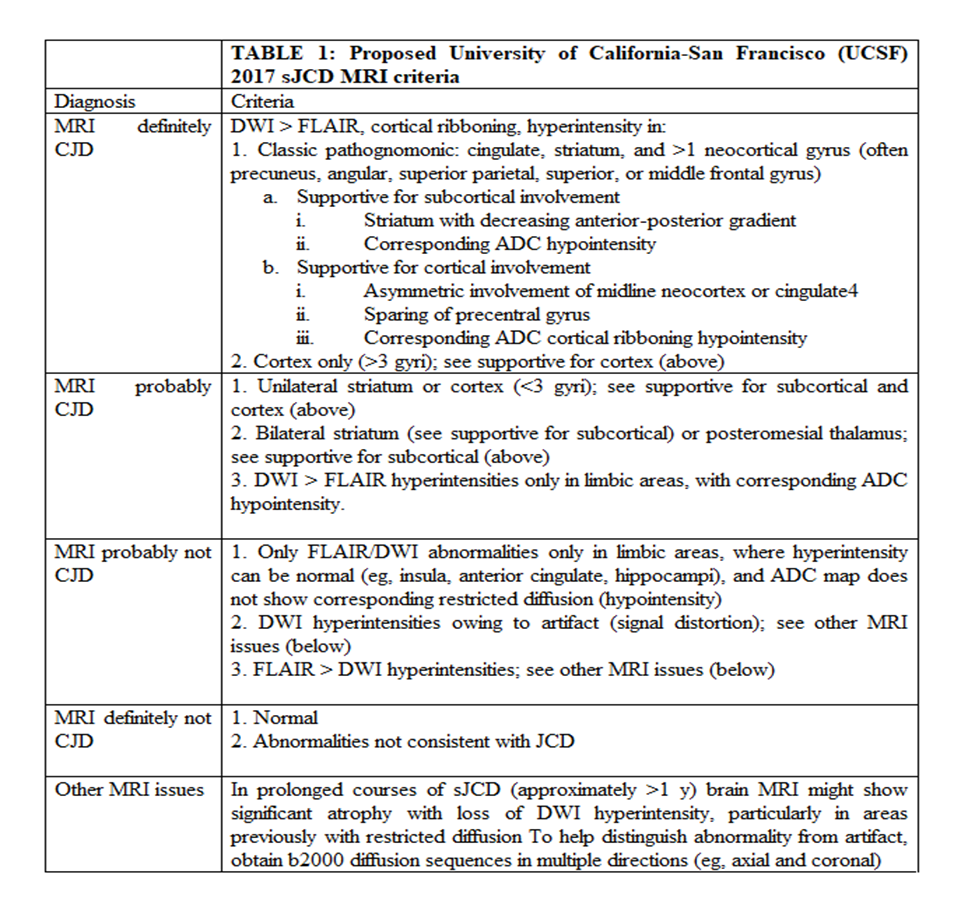
In addition, the workup of dementia in this case was consistant with sCJD. Her CSF analysis showed high protiens content but specific biomarkers was not performed. CSF protien content indicates rapid neuronal damage [2]. Certain protein biomarkers have shown to have high sensitivity for CJD such as 14-3-3 protein, neuron-specific enolase (NSE), total-tau (t-tau), and S100ß, yet, they should not be used solely for diagnosis as they could be found in other neurological condition like stroke, multiple sclerosis, brain tumors, Alzheimer’s disease, or frontotemporal dementia [2]. Periodic sharp-wave complexes on EEG has a high specificity especially as the disease advances [2]. Lastly, we confirmed our diagnosis from MRI brain findings that were compatible with definitive diagnosis of CJD as per The University of California–San Francisco (UCSF) classification (see table 1). Our lady showed asymmetrical cortical ribbon in the parietal, occipital cortex, cingulate gyrus, and left neocortex. Hyper-intensity represents vacuolation and PrPsc deposition and they are better detected in DWI and ADC rather than in FLAIR [1,2].Of note, the involvement of anatomical areas in MRI could guide to recognize the type, and anticipate the duration of illness eg, hyper-intensities in DWI of the occipital cortex correlates to a short disease spectrum from the initial symptoms to death [1]. Perhaps the occipital lobe affection in this lady hastened her death. Brain biopsy remains the gold standard for the diagnosis, but we had not performed it as it has a low sensitivity, and such an invasive method would not alter the disease prognosis [1]. The advance improvement in imaging modalities and other emerging test like real-time quaking-induced conversion assay (RT-QuIC) have been proven to be of a high diagnostic accuracy in detecting CJD and spare the need for brain biopsy [1,2].
Given the high consumption of meat products in the dietary history of our deceased lady, we have done a wide search on literature to find a link between sCJD and certain food component. PrPsc is abundant in the brain given the fact that prion is a normal protein of the brain, but it has also been found in other tissues such as stomach, intestine, muscles, and the lymphatic system [4]. Animal muscles are the most consumed dietary component and were found to have the infectious prion to a lesser than 5,000 times than in the brain [4]. Generally, the infectious form has many hosts including sheep, goat, pigs, chicken, and even certain kind of fishes [4]. Between 1991 to 1993, Davanipour et al studied dietary risk factors for development of CJD in 11 state in the United State of America (USA) and found that consumption of certain food whether in low or high quantities were statistically significant to the development of sCJD [4]. These items encompass wide ranges of food such as processed food, hot dogs, sausage, pepperoni, kielbasa, canned meat, poultry liver, any stomach/intestine, beef stomach/intestine, and other organ tissue. However, this study showed no increased risk with brain content consumption [4].Between 1993-1995, Van Duijn et al, conducted a large study in 6 European countries and concluded that brain content, raw meat and pork are associated with increase risk to develop |CJD [5]. However, there was over 70% missing data of the cases and controls about the brain and raw fish consumption and after another analysis the author stated that brain consumption was no longer significant [4]. Perhaps cooking condition could participate in transmitting the infectious prion form as per Goldberg et al. study who pointed that brain eater preferred light grilling which does not provide heat to kill the abnormal prion protien [4].
Our case was a lady in an advanced age, who used to consume large quantity of meat products through her life, died in a very brief time frame from the initial presentation of symptoms. Within 40 days, her symptoms evolved rapidly from constitutional symptoms followed by progressive dementia, then death. EEG and MRI findings were classic of sCJD. The brain biopsy was not done, and the new diagnostic facilities is not available in our country. We would like to share this case to raise the awareness of the meat products could jeopardize people’ life as they are the host for this killing mutated protein form.