AUCTORES
Globalize your Research
Research Article | DOI: https://doi.org/10.31579/2637-8892/022
*Corresponding Author: Dott. Giulio Perrotta
Citation: Giulio Perrotta, The Phenomenon of Demonic Possession: Definition, Contexts and Multidisciplinary Approaches. J. Psychology and Mental Health Care. 3(2) . DOI: 10.31579/2637-8892/022
Copyright: © 2019 Giulio Perrotta, This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium,provided the original author and source are credited.
Received: 28 June 2019 | Accepted: 17 July 2019 | Published: 22 July 2019
Keywords: anxiety disorders; panic attack; panic disorder; nightmares; sleepwalking; sex in sleep; nocturnal paralysis; hallucinations; nocturnal awakenings; awakening; narcolepsy; hypersomnia; amygdala; prefrontal
Starting from the macro-category "sleep-wake disorders", as defined in DSM-V, the individual pathological conditions were defined, focusing on the contextual and clinical aspects, to continue the analysis on neural correlates and strategic therapy to be used to solve the problems encountered.
1. Introduction. Sleep: definition and contexts [1]
The sleep [2] is defined as a state of rest opposed to waking. Various definitions indicate sleep as "a periodic suspension of the state of consciousness"; during which the body recovers energy; state of physical and mental rest; characterized by the temporary detachment of the conscience and the will; by the slowing down of the neurovegetative functions and by the partial interruption of the subject's sensorimotor relationships with the environment; indispensable for the restoration of the organism." [3] Like waking; in fact; sleep is an active physiological process that involves the interaction of multiple components of the central and autonomic nervous system. In fact; although sleep is represented by an apparent state of rest; during this state complex changes take place in the brain that cannot be explained only as a simple state of physical and mental rest. For example; there are some brain cells that at some stages of sleep have an activity 5-10 times greater than what they are awake. [4]
Two fundamental characteristics distinguish sleep from the waking state: the first is that in sleep a perceptive barrier is created between the conscious world and the external world; the second is that a sensory stimulus of a certain level (for example a loud noise) can overcome this barrier and make the sleeping person wake up.
Proper sleep is biologically imperative for sustaining life. The psychophysical health of the individual depends on the quality and duration of sleep. Sleep disorders; such as insomnia; are present in many psychiatric disorders; in which sleep deprivation has a significant impact on a person's quality of life.
It is difficult to give a precise and unambiguous definition of sleep. One of the most apt is the one given in 1985 by Fagioli and Salzarulo; who present it as "a state of the organism characterized by reduced reactivity to environmental stimuli that involves a suspension of relational activity (relationships with the environment) and modifications of the state of consciousness: it is established autonomously and periodically; is self-limited in time and is reversible ".
Another well accepted definition defines it as "a temporary and reversible detachment of the mind from the body; indispensable for the proper functioning of both". [5]
Yet another definition indicates it as: "A readily reversible state of reduced activity and interaction with the surrounding environment." Thus the term "readily reversible" cannot be associated with coma or anesthesia which; respectively; are a pathology and a pharmacologically induced state of rest.
Sleep therefore differs from other states of altered consciousness:
a) with sleep the abolition of the state of vigilance is; as already mentioned; reversible. Thus the subject can awaken after an even painless stimulus;
b) otherwise; stupor is an alteration of the state of consciousness from which one can awaken only after administering a painful stimulus;
c) the comatose state is an alteration of the state of consciousness from which one cannot awaken after administering a painful stimulus;
d) brain death is much more serious with the irreversible cessation of all brain activity.
Traditionally; three main measures have been used to define sleep physiology:
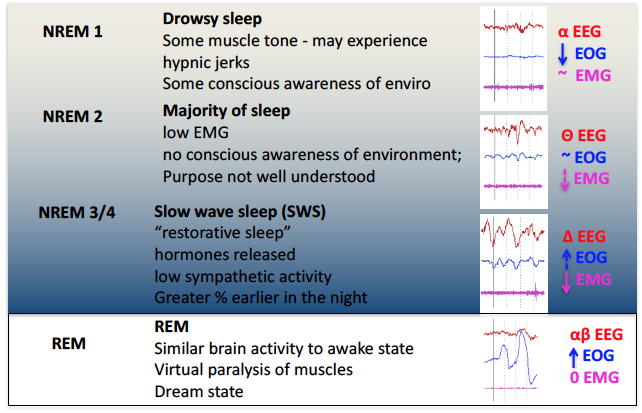
In 1953; Eugene Aserinsky and Nathaniel Kleitman discovered the presence of rapid eye movements (REM) during sleep. This simple observation made it possible to differentiate sleep in a REM phase (with rapid eye movements) and in a non-REM phase (NREM phase). In 1963; Kleitman and Dement described for the first time the alternation; during the period of sleep; of REM and NREM sleep in cycles; introducing the concept of sleep architecture. At the end of the 1960s; after the discovery of REM and NREM sleep and the concept of cyclical nature of these two phases within sleep; the need arose to classify the electroencephalographic changes that occurred during sleep in a macroscopic manner in a standard manner. In 1968; Rechtschaffen and Kales based on the analysis of electroencephalographic; electromyographic and electrooculographic parameters classified sleep in 5 stages: 4 NREM stages (stage 1; stage 2; stage 3; stage 4) and a REM stage.
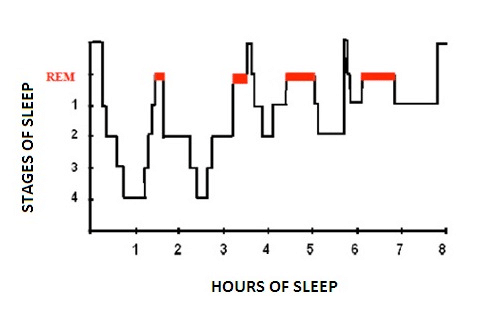
1. Hypnogram.
Sleep presents a regular alternation of non-REM and REM phases consisting of cycles of similar duration to each other. After falling asleep the subject progressively passes from stage 1 of non-REM sleep to stage 2; after which he passes to stage 3 or stage 4 and then; between 70 and 90 minutes after falling asleep; the first phase of REM sleep occurs which lasts about 15 minutes. At the end of the first phase of REM sleep the first cycle ends; which lasts approximately 80 to 100 minutes.
After the first cycle; others of a rather constant duration follow one another; but where REM sleep tends to increase in duration at the expense of non-REM sleep; in particular stages 3 and 4 (deep sleep) which become shorter. During the night; in the end; REM sleep constitutes about 25% of the total sleep duration. It is possible that there are waking moments between the various cycles. The period of sleep is represented graphically by the hypnograms that illustrate the succession of the phases of wakefulness and sleep in relation to time. Today in place of the subdivision into four stages the nomenclature in three phases (N1; N2 and N3) adopted by the American Academy of Sleep Medicine in 2007 on the basis of the appearance and frequencies of the EEG oscillations; in which phase N3 combines stages 3 and 4 both characterized by the same large slow waves; even if in different percentages.
During the vigil; the EEG basically alternates between two patterns. A pattern called "activation" (or desynchronized pattern) characterized by low voltage waves (10-30 microvolts) and high frequency (16-25 Hz) and a second called "alpha activity" characterized by sine waves of 8-12 Hz Alpha activity is typically present and abundant when the subject is relaxed with eyes closed. The activation pattern is present when the patient is in a state of attention with open eyes. Eye movements are both rapid and slow and muscle tone is medium to high.
During stage 1; the alpha activity decreases; the activation pattern is poor and the EEG consists mainly of low-voltage waves of mixed frequency between 3-7 Hz. The movements of the eyes are still present but slow; rotating and oscillators (not in phase opposition as in the REM phase). The electromyogram shows a persistent tonic activity although of a lower intensity than the wake. In stage 2 there is a relatively low background activity; with variable frequency but close to theta waves (3–7 Hz). Stage 2 is characterized by the presence of two components; the so-called K complexes and the spindles of sleep (or spindles). The latter of thalamic origin; lacking in lethal family insomnia; a deadly disease for sleep deprivation. The eye movements are slow; while the EMG is further reduced. In stage 3; 20% - 50% of each epoch (conventionally an EEG recording period of 30 s) must contain Delta activities; ie large amplitude EEG waves (> 75 microvolts) and low frequency (about 0.5 - 4 Hz). The muscle tone in this stage is slightly reduced and the eye movements practically absent. The spindles of sleep may or may not occur; while the K complexes are present; although they are often difficult to distinguish from delta waves. Stage 4 is characterized by the presence of delta waves; which here reach the maximum amplitude and minimum frequency; for more than 50% of each era. As for stage 3; the spindles can be absent or present while the K complexes are present; but almost unrecognizable from the underlying delta rhythm. The movements of the eyes are not present while a state of very low tonic muscle activation persists. At this stage the metabolic activity of the brain is reduced (lower consumption of oxygen and glucose). If the subject wakes up at this stage he can get confused for a few minutes.
2. Sleep phisiology. Part I. Source: https://foreverfitscience.com/sleep/sleep-physiology/

3. Sleep phisiology. Part II. Source: https://healthengine.com.au/info/sleep-physiology

4. Sleep phisiology. Part III. Source: https://www.slideshare.net/mabdelghani/physiology-of-sleep-and-eeg-for-undergraduates
The REM stage is characterized by a low voltage EEG with mixed frequencies. The EEG of REM sleep is very reminiscent of that of stage 1 if not for the discharged characteristics of waves with the characteristic 'saw-tooth' morphology. PGO (ponto-genic-occipital) waves appear; the activity of the hippocampus becomes synchronized with the appearance of theta waves. The stadium takes its name from rapid eye movements and the low tone of the mental muscles. Moreover; this phase is characteristic for the paralysis of the muscles (to avoid mimicking dreams) and because it is the one in which dreams predominantly occur. The brain consumes oxygen and glucose as if the subject were awake and engaged in intellectual activity. If you wake up in this phase you are perfectly oriented. This stage is also characterized by a more imprecise control of the vegetative functions of the organism; in fact the arterial pressure increases and undergoes sudden changes; the heart rate increases and extrasystoles can appear; the respiratory frequency becomes more irregular and the part is compromised thermoregulation. Penile erection in men and genital changes in women may occur. REM sleep tends to decrease with advancing age and reaches a peak at the age of 1 year and then decreases in favor of non-REM sleep.
Sleep deprivation was tested by Randy Gardner in 1965; a young 17-year-old student who stayed awake for 264 hours; or 11 days. On the second day; his concentration diminished and subsequently lost the ability to identify objects by touch. At the end of the third day he experienced bad temper and disorientation. At the end of the experiment it was difficult to concentrate; to remember recent events; he became paranoid and began to hallucinate. On the eleventh day; the medical personnel who kept him under control wrote: "Confusional state and disorientation; sudden mood swings; irritability; speak with a road sign believing him a man; hallucinations; temporary loss of identity; difficulty in pronouncing tongue twisters; mumbles many words; diminished reflexes; memory lapses; difficulty in focusing objects; visual problems with too bright colors ... ". When we sleep little; in fact; learning; memory; mood and quick reflexes are compromised. Several studies show that sleeping systematically less than six hours a night increases the risk of heart attack for well over four and a half times compared to those who sleep regularly.
2. Sleep-wake disorders: classification and clinical contexts [6]
When we talk about these disorders we refer to a wide range of problems characterized by an alteration of the sleep-wake rhythm. Those who present these disorders are unable to benefit from their rest and perceive their sleep as insufficient or unsatisfactory in quality and quantity; resulting in stress and discomfort during waking hours.
Due to the close connection between sleep quality and physical and emotional health; even when a sleep disorder occurs occasionally in a person; it should never be neglected. Sleep-related disorders are accompanied by clinically significant distress or impairment in the social; occupational or other important areas.
Sleep-wake disorders include the following sub-categories with related symptoms:
1) Insomnia disorder: predominant dissatisfaction with the quantity or quality of sleep associated with difficulty in starting sleep at bedtime; maintaining sleep; with frequent or prolonged awakenings during the night and early morning awakening with difficulty go back to sleep. For there to be a diagnosis of insomnia disorder the difficulty of sleeping must occur at least 3 times a week and must persist for at least three months despite adequate sleeping conditions.
2) Hypersomnolence disorder: excessive sleepiness despite a main sleep period of at least 7 hours; manifesting at least three times a week for at least three months. It is accompanied by clinically significant distress or impairment in cognitive; social; occupational or other important areas. It is not attributable to the effects of a substance (a substance of abuse; a drug) and the complaint of sleepiness is not adequately explained by the coexistence of mental and clinical disorders. It is not justified by another sleep disorder and does not occur exclusively during the course of another sleep disorder.
3) Narcolepsy: it is characterized by recurrent periods of irrepressible bi-dream of sleeping; sleep attacks or naps that occur on the same day. These episodes must have occurred at least three times a week in the last 3 months. In order for there to be a diagnosis of narcolepsy; episodes of cataplexy must occur at least a few times a month; characterized by a sudden; brief and reversible episode of muscle weakness that occurs in conjunction with emotional stimuli; such as laughter; surprise; anger; joy or sadness.
4) Respiratory-related sleep disorders:
a) Obstructive sleep apnea / hypopnea: repeated episodes of obstruction of the upper airway (pharyngeal) during sleep that can manifest itself with nocturnal respiratory disorders or daytime sleepiness; asthenia or non-restorative sleep despite sufficient opportunity to sleep and not explained by other mental disorder or medical condition. Furthermore it is necessary that there are polysomnographic evidences of 15 or more apnea and / or obstructive hypopneas per hour of sleep.
b) Central sleep apnea: repeated episodes of apnea and hypopnea during sleep caused by a change in respiratory effort. These are ventilation control disorders in which respiratory events occur with a periodic or intermittent pattern. This disorder is detectable when polysomnographic evidences of 5 or more central apnea are present per hour of sleep and when the disorder is not better explained by another concomitant sleep disorder.
c) Sleep-related hypoventilation: polysomnography shows episodes of decreased respiration associated with high levels of carbon dioxide; in the absence of a concomitant sleep disorder.
5) Circadian disorders of the wake-sleep rhythm: sleep interruption due to an alteration of the circadian system; to a misalignment of the endogenous circadian rhythm and the wake-sleep rhythm required by the physical conditions of an individual or imposed by social or work commitments. In these cases; sleep interruption leads to excessive sleepiness or insomnia or both. Sleep disturbance causes clinically significant distress or impairment in social; occupational or other important areas.
a) Confusionale wake up. Episodes of partial awakening not associated with walking or autonomic disorders (the child seems to be awake but confused; disoriented; sometimes aggressive; does not respond adequately to orders; can speak but not in an inconsistent way);
b) Sleepwalking. Episodes characterized by more or less complex automatic behavior (like walking; eating; drinking; leaving home ...);
c) Night terrors. Episodes of partial awakening; often with sudden onset; with expression of terror; intense agitation; sweating; pallor; wheezing; tachycardia.
They are complex motor manifestations that occur during REM sleep:
a) Behavioral disorder in REM.
REM sleep represents that phase of sleep; mostly represented in the second part of the night; in which there is an almost complete loss of tone of the voluntary musculature ("it is as if immobilized") and during which the more dreamlike activity occurs intense. The behavioral disturbance in REM sleep (RBD) is characterized by the loss of physiological muscle atony. For this reason; during the episodes; which occur more frequently in the second part of the night; the patients present an excessive motor activity; often characterized by abrupt behavior (such as screaming; punching and kicking); in relation to the content of their dreams. In fact; patients often report dreams with a negative content; which they "act" by performing violent actions; which can assume characteristics of aggressiveness; for example towards the bed partner. These manifestations therefore entail a high risk of trauma both for the patient and for those close to him. Their duration is usually between 2 and 10 minutes and the frequency can be very varied: from weekly or monthly episodes to multi-night (4-5 / night).
b) Sleep paralysis.
They consist in the inability to perform any voluntary motor activity (one has the perception of being completely immobilized); although the subject is completely conscious. They can occur during the phase of falling asleep ("hypnagogic paralysis") or following an awakening ("hypnopompic paralysis"). They can be accompanied by auditory or visual hallucinations and can last from a few seconds to several minutes; often causing intense anxiety in the person who lives them. They can be resolved spontaneously or following sensory stimulation. They can be favored by an irregular sleep-wake rhythm and sleep deprivation.
c) Nightly nightly.
They consist of fearful dreams; with a negative content; often of long duration; these dreams frequently induce the awakening of the subject that keeps a vivid memory of it. They are common in children or in patients with "post-traumatic stress disorder". They can be favored by fever or by the abrupt withdrawal of alcohol or drugs that reduce REM sleep (amphetamines; some antidepressants and benzodiazepines). These conditions; in fact; could lead to a sharp and significant increase in the representation of REM sleep; favoring the occurrence of nightmares.
It consists of the emission of a monotonous vocalization during a prolonged exhalation associated with bradypnea (reduction of respiratory rate). It often arises at a young age (20-30 years). The episodes; which last about 2-20 seconds; occur more frequently during REM sleep (especially in the second half of the night). The cause still appears to be unknown and; at present; there is no treatment. Cases have been described in association with sleep apnea and only a few have been resolved with nocturnal ventilatory treatment. However; it is important to distinguish such manifestations from snoring episodes.
It is characterized by the perception of a sound often very intense; similar to an explosion or an explosion; which occurs especially during the phase of falling asleep; often resulting in a sudden awakening. The perceived sound; although very violent; is never accompanied by pain; but sometimes it can be related to visual flashes. If the crises are recurrent and the sound perceived is particularly intense; the patient will tend to fall asleep with fatigue for fear of a new attack. The syndrome affects mainly women around the age of 50 and can be favored by stressful conditions. Currently there is no univocal explanation of these phenomena as well as an effective therapy (some cases described have been treated with calcium channel blockers).
Vivid experiences; similar to dreams; often with bizarre or terrifying contents; which occur during sleep ("hypnagogic") or after awakening ("hypnopompic"). During the attacks the fantastic sensations can be mistaken for real. In most cases these are visual hallucinations; but they can also be auditory; tactile; gustatory or olfactory. They may be associated with sleep paralysis and; like these; occur frequently in individuals without other sleep disorders or may be one of the symptoms of narcolepsy.
Consists of repeated episodes during sleep of compulsive food or drink ingestion (even unusual or inedible); often the level of consciousness during the episodes appears to be null or partial; just as the patient on waking frequently does not retain any memory of what happened. This form of parasomnia appears more frequent in the female sex and has an onset around the 20-30 years; familiarity with other NREM sleep parasomnias is common. SRED can be associated with other sleep disorders (arousal disorders; restless legs syndrome; sleep apnea; narcolepsy) and can be triggered by taking certain drugs (benzodiazepines; zolpidem; lithium) or by abrupt withdrawal of alcohol intake. This syndrome must be distinguished from other forms of eating behavior in sleep such as "Night Eating Syndrome"; characterized by hyperphagia (overeating) evening and night and / or anorexia (lack of appetite) morning and insomnia.
3. The neural correlates in sleep-wake disorders [7]
A first system that controls and maintains the waking state is represented by the aminergic nuclei of the brainstem; in particular by the noradrenergic neurons of the locus coeruleus and by the serotonergic neurons of the raphe nuclei; but it is assumed that the substance dopaminergic neurons also play a role Black. These neurons project diffusely to the cortex; the thalamus; the hypothalamus and the hippocampus. When the subject is alert; the discharge frequency of the neurons of these systems is maximum; is greatly reduced during non-REM sleep and almost completely during REM sleep; suggesting that they are systems involved in waking maintenance. These neurons can also undergo phenomena of self-inhibition that promote sleep. Conditions that stimulate activity promote wakefulness; but if these systems are inhibited; sleep is promoted. If; however; it seems true that the stimulation of the noradrenergic system stimulates and maintains wakefulness; serotonin; while also stimulating wakefulness; favors; over time; the synthesis and release of substances that promote sleep and inhibit the cholinergic neurons of the forebrain basal; involved in maintaining the vigil; thus playing an ambiguous role.
A second system that promotes wakefulness is the cholinergic neurons of the basal forebrain. These neurons project to the cortex; activating it; to the hippocampus and amygdala; and; in addition to being awake; they are active during the REM phase; which are not very active in the non-REM phase. They are inhibited by serotoninergic terminations originating from the raphe nuclei. The cholinergic nuclei of the brainstem include the laterodorsal nucleus of the pontine tegmentum and the peduncolopontine tegmentum nucleus which are made up of two populations of neurons. A first population is characterized by neurons active during REM sleep; which discharge at very low frequency during wakefulness and non-REM sleep and which project to the aminergic nuclei of the brainstem. The second population consists of neurons whose discharge frequency is maximum during wakefulness and during REM sleep and which project to the thalamus and hypothalamus; activating them. The tuberomammillary nucleus contains histaminergic hypothalamic neurons which project diffusely to almost the entire central nervous system; promoting waking maintenance and are maximally active in this phase. The inhibition of these neurons with antihistamine induces sleepiness. The posterolateral hypothalamus comprises a small group of orexinergic neurons that maintain vigil and are also involved in the regulation of food intake. They diffusely project to the structures involved in the regulation of the sleep-wake cycle in the central nervous system.
Vigil is a behavioral state characterized by arousal and cortical activation; manifested in a desynchronized EEG pattern. In humans it is characterized by a beta-type rhythm (frequency: 15 - 30 Hz; amplitude: <20 µV) during active and alpha-type vigil (frequency: 8 - 12 Hz; amplitude: < 50 µV) during a relaxed vigil.
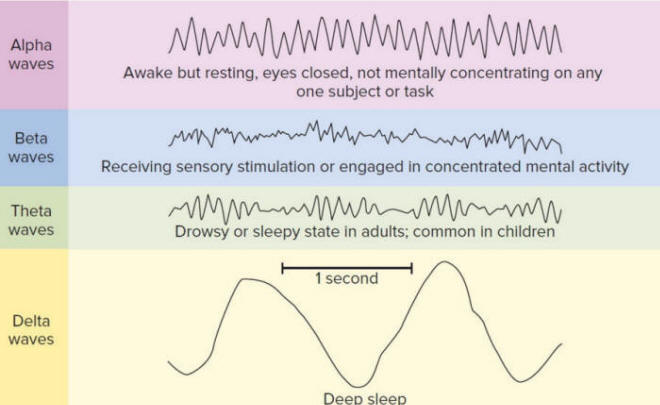
5. Sleep waves. Source: https://corrosion-doctors.org/Dreaming%20is%20Personal/Glossary.htm
This behavioral state is supported by the interaction between different brain regions and by different types of neuromedicators:
4. Melatonin: contexts and clinical profiles [8]
From a neurobiochemical point of view; as already stated; the pineal gland produces melatonin; a hormone isolated for the first time in 1958 by Aaron Lerner and produced by pinealocytes starting from the neurotransmitter serotonin (5-hydroxy-tryptamine) for N-acetylation and oxy-methylation; by virtue of the fact that these cells contain the enzyme hydroxy- indole-oxy methyl transferase (HIOMT); epiphysis marker enzyme.
It acts in the circadian rhythm of sleep and has powerful antioxidant effects: melatonin is synthesized in the absence of light from the pineal gland; shortly after the onset of darkness; its concentrations in the blood increase rapidly and reach the maximum between 2 and 4 am and then gradually decrease as the morning approaches.
Exposure to light (especially at the blue wavelength between 460 and 480 nm) inhibits the production of melatonin in a dose-dependent manner. It is therefore used for the short-term treatment of insomnia over 55 years of age.
The side effects of melatonin are not null; although the contrary belief is widespread: over the years; various professional bodybuilders and various sports information magazines have affirmed the possibility; with the support of some scientific studies; that daily doses between 0.5 mg and 3 mg; taken 30-60 minutes before training; increase the levels of growth hormone; without giving side effects; which are usually recognized in irritability and drowsiness.
Melatonin decreases the release of GnRH: for this reason the synthesis of testosterone and therefore libido decreases. More precisely; it inhibits the secretion of the luteinizing hormone; which stimulates the male endocrine activity of the interstitial cells of the testis with testosterone and sperm production; and in the female ovulation and conversion of the ovarian follicle into the corpus luteum. Taken for prolonged periods; melatonin can have a depressive effect in predisposed subjects; furthermore; it can inhibit ovulation precisely because of the suppression of the GnRH release it causes.
Recent research in the biomedical field; especially on melatonin; has shown that:
1) melatonin is importantly involved in inflammatory processes and cellular apoptosis. [9]
2) exposure to electromagnetic fields decreases the secretion of melatonin [10]; which negatively affects cellular processes linked to death; acts on sex hormones and connected glands and interferes with the sleep-wake rhythm. [11]
3) melatonin intervenes in the neurobiological processes involved in anorexic and bulimic disordersand in the predisposition to be subject to these psychophysical pathologies. [12]
4) melatonin is involved with cortisol in the immunomodulatory response. [13]
5) melanin intervenes in the regulation of acidosis in malignant tumor processes. [14]
6) melatonin is a potent inhibitor of ovarian [15] and prostate cancer. [16]
7) melatonin has positive effects on blood pressure; reducing hypertension. [17]
8) melatonin; having antioxidant and modulating properties of the circadian rhythm; has positive effects on drug therapy in the presence of schizophrenia [18] and in general in psychotic syndromes. [19]
9) melatonin has a positive effect on blood sugar; reducing blood levels and favoring a positive prognosis on insulinic therapy in the rats. [20]
10) melatonin; compared to problems related to the central nervous system; seems to be directly involved in the reduction of tissue and nerve lesions; affecting free radicals due to its powerful antioxidant effect. Since endogenous melatonin levels decrease significantly in senility; these results imply that the loss of this antioxidant could contribute to the incidence or severity of some age-related neurodegenerative diseases. [21]
11) melatonin; precisely because it is related to serum and ionized calcium levels [22]; positively intervenes in vertebral disorders [23] and intervertebral degeneration (in chicken) [24]; also in the cartilaginous problems [25] and curvature of scoliosis. [26]
12) melatonin has beneficial effects on respiratory problems linked to obstructive bronchospasm. [27]
In recent decades [28] [29]; the integration of melatonin in the diet has allowed a significant and positive management of primary sleep disorders; especially at a dose of 2 - 10 mg; unlike the classic 0;5 - 1 mg dose indicated for jet lag disorder.
5. Conclusions
Sleep disorders represent a primitive alteration of its regulatory mechanisms and therefore of the physiological rhythms of the sleep-wake cycle or be the clinical expression of other pathologies; organic or psychic. Chronic sleep deprivation; altering the sleep-wake cycle e all the associated biological rhythms; involves the exhaustion of energy that feeds our life; compromising its quality in all its dimensions: personal; affective; family; socio-relational and working. Sleep is therefore a cornerstone of health.
For this reason; morphological disorders must always be taken seriously consideration and shared with your doctor to be able to identify and therefore eliminate; where possible; any causes triggers; through a targeted behavioral and / or intervention pharmacological. The so-called "sleep hygiene"; which is achieved through the adoption of behaviors that aim to promote a good night's sleep; already helps improve sleep quality and maintain it over time; representing the primary strategy.
The basic advice; in the absence of diseases; to sleep properly are:
- Respect your own sleep-wake rhythm; lying down and waking up around the same time (even during the weekend) and avoiding naps during the day.
- Always follow the same ritual before going to bed; dedicating yourself to relaxing activities.
- Perform physical activity during the day and not in the evening hours.
- Take meals at regular times; preferring a light diet for dinner.
- Avoid the intake of exciting substances (tea; coffee; alcohol; nicotine) in the evening hours.
- Rest on a comfortable bed in a cool; dark room silent and well ventilated.
In the presence of a pathological disorder; however; the intervention of a specialist in neurology or psychiatry is required to carry out a targeted therapy consisting of pharmacological and / or psychotherapeutic treatment.
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.
Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.

This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!
"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.
Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.
Clinical Cardiology and Cardiovascular Interventions I testity the covering of the peer review process, support from the editorial office, and quality of the journal.

Clinical Cardiology and Cardiovascular Interventions, we deeply appreciate the interest shown in our work and its publication. It has been a true pleasure to collaborate with you. The peer review process, as well as the support provided by the editorial office, have been exceptional, and the quality of the journal is very high, which was a determining factor in our decision to publish with you.
The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews journal clinically in the future time.
Clinical Cardiology and Cardiovascular Interventions, I would like to express my sincerest gratitude for the trust placed in our team for the publication in your journal. It has been a true pleasure to collaborate with you on this project. I am pleased to inform you that both the peer review process and the attention from the editorial coordination have been excellent. Your team has worked with dedication and professionalism to ensure that your publication meets the highest standards of quality. We are confident that this collaboration will result in mutual success, and we are eager to see the fruits of this shared effort.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, I hope this message finds you well. I want to express my utmost gratitude for your excellent work and for the dedication and speed in the publication process of my article titled "Navigating Innovation: Qualitative Insights on Using Technology for Health Education in Acute Coronary Syndrome Patients." I am very satisfied with the peer review process, the support from the editorial office, and the quality of the journal. I hope we can maintain our scientific relationship in the long term.
Dear Monica Gissare, - Editorial Coordinator of Nutrition and Food Processing. ¨My testimony with you is truly professional, with a positive response regarding the follow-up of the article and its review, you took into account my qualities and the importance of the topic¨.

Dear Dr. Jessica Magne, Editorial Coordinator 0f Clinical Cardiology and Cardiovascular Interventions, The review process for the article “The Handling of Anti-aggregants and Anticoagulants in the Oncologic Heart Patient Submitted to Surgery” was extremely rigorous and detailed. From the initial submission to the final acceptance, the editorial team at the “Journal of Clinical Cardiology and Cardiovascular Interventions” demonstrated a high level of professionalism and dedication. The reviewers provided constructive and detailed feedback, which was essential for improving the quality of our work. Communication was always clear and efficient, ensuring that all our questions were promptly addressed. The quality of the “Journal of Clinical Cardiology and Cardiovascular Interventions” is undeniable. It is a peer-reviewed, open-access publication dedicated exclusively to disseminating high-quality research in the field of clinical cardiology and cardiovascular interventions. The journal's impact factor is currently under evaluation, and it is indexed in reputable databases, which further reinforces its credibility and relevance in the scientific field. I highly recommend this journal to researchers looking for a reputable platform to publish their studies.

Dear Editorial Coordinator of the Journal of Nutrition and Food Processing! "I would like to thank the Journal of Nutrition and Food Processing for including and publishing my article. The peer review process was very quick, movement and precise. The Editorial Board has done an extremely conscientious job with much help, valuable comments and advices. I find the journal very valuable from a professional point of view, thank you very much for allowing me to be part of it and I would like to participate in the future!”

Dealing with The Journal of Neurology and Neurological Surgery was very smooth and comprehensive. The office staff took time to address my needs and the response from editors and the office was prompt and fair. I certainly hope to publish with this journal again.Their professionalism is apparent and more than satisfactory. Susan Weiner

My Testimonial Covering as fellowing: Lin-Show Chin. The peer reviewers process is quick and effective, the supports from editorial office is excellent, the quality of journal is high. I would like to collabroate with Internatioanl journal of Clinical Case Reports and Reviews.

My experience publishing in Psychology and Mental Health Care was exceptional. The peer review process was rigorous and constructive, with reviewers providing valuable insights that helped enhance the quality of our work. The editorial team was highly supportive and responsive, making the submission process smooth and efficient. The journal's commitment to high standards and academic rigor makes it a respected platform for quality research. I am grateful for the opportunity to publish in such a reputable journal.
My experience publishing in International Journal of Clinical Case Reports and Reviews was exceptional. I Come forth to Provide a Testimonial Covering the Peer Review Process and the editorial office for the Professional and Impartial Evaluation of the Manuscript.

I would like to offer my testimony in the support. I have received through the peer review process and support the editorial office where they are to support young authors like me, encourage them to publish their work in your esteemed journals, and globalize and share knowledge globally. I really appreciate your journal, peer review, and editorial office.
Dear Agrippa Hilda- Editorial Coordinator of Journal of Neuroscience and Neurological Surgery, "The peer review process was very quick and of high quality, which can also be seen in the articles in the journal. The collaboration with the editorial office was very good."

I would like to express my sincere gratitude for the support and efficiency provided by the editorial office throughout the publication process of my article, “Delayed Vulvar Metastases from Rectal Carcinoma: A Case Report.” I greatly appreciate the assistance and guidance I received from your team, which made the entire process smooth and efficient. The peer review process was thorough and constructive, contributing to the overall quality of the final article. I am very grateful for the high level of professionalism and commitment shown by the editorial staff, and I look forward to maintaining a long-term collaboration with the International Journal of Clinical Case Reports and Reviews.
To Dear Erin Aust, I would like to express my heartfelt appreciation for the opportunity to have my work published in this esteemed journal. The entire publication process was smooth and well-organized, and I am extremely satisfied with the final result. The Editorial Team demonstrated the utmost professionalism, providing prompt and insightful feedback throughout the review process. Their clear communication and constructive suggestions were invaluable in enhancing my manuscript, and their meticulous attention to detail and dedication to quality are truly commendable. Additionally, the support from the Editorial Office was exceptional. From the initial submission to the final publication, I was guided through every step of the process with great care and professionalism. The team's responsiveness and assistance made the entire experience both easy and stress-free. I am also deeply impressed by the quality and reputation of the journal. It is an honor to have my research featured in such a respected publication, and I am confident that it will make a meaningful contribution to the field.

"I am grateful for the opportunity of contributing to [International Journal of Clinical Case Reports and Reviews] and for the rigorous review process that enhances the quality of research published in your esteemed journal. I sincerely appreciate the time and effort of your team who have dedicatedly helped me in improvising changes and modifying my manuscript. The insightful comments and constructive feedback provided have been invaluable in refining and strengthening my work".

I thank the ‘Journal of Clinical Research and Reports’ for accepting this article for publication. This is a rigorously peer reviewed journal which is on all major global scientific data bases. I note the review process was prompt, thorough and professionally critical. It gave us an insight into a number of important scientific/statistical issues. The review prompted us to review the relevant literature again and look at the limitations of the study. The peer reviewers were open, clear in the instructions and the editorial team was very prompt in their communication. This journal certainly publishes quality research articles. I would recommend the journal for any future publications.

Dear Jessica Magne, with gratitude for the joint work. Fast process of receiving and processing the submitted scientific materials in “Clinical Cardiology and Cardiovascular Interventions”. High level of competence of the editors with clear and correct recommendations and ideas for enriching the article.

We found the peer review process quick and positive in its input. The support from the editorial officer has been very agile, always with the intention of improving the article and taking into account our subsequent corrections.

My article, titled 'No Way Out of the Smartphone Epidemic Without Considering the Insights of Brain Research,' has been republished in the International Journal of Clinical Case Reports and Reviews. The review process was seamless and professional, with the editors being both friendly and supportive. I am deeply grateful for their efforts.
To Dear Erin Aust – Editorial Coordinator of Journal of General Medicine and Clinical Practice! I declare that I am absolutely satisfied with your work carried out with great competence in following the manuscript during the various stages from its receipt, during the revision process to the final acceptance for publication. Thank Prof. Elvira Farina

Dear Jessica, and the super professional team of the ‘Clinical Cardiology and Cardiovascular Interventions’ I am sincerely grateful to the coordinated work of the journal team for the no problem with the submission of my manuscript: “Cardiometabolic Disorders in A Pregnant Woman with Severe Preeclampsia on the Background of Morbid Obesity (Case Report).” The review process by 5 experts was fast, and the comments were professional, which made it more specific and academic, and the process of publication and presentation of the article was excellent. I recommend that my colleagues publish articles in this journal, and I am interested in further scientific cooperation. Sincerely and best wishes, Dr. Oleg Golyanovskiy.

Dear Ashley Rosa, Editorial Coordinator of the journal - Psychology and Mental Health Care. " The process of obtaining publication of my article in the Psychology and Mental Health Journal was positive in all areas. The peer review process resulted in a number of valuable comments, the editorial process was collaborative and timely, and the quality of this journal has been quickly noticed, resulting in alternative journals contacting me to publish with them." Warm regards, Susan Anne Smith, PhD. Australian Breastfeeding Association.

Dear Jessica Magne, Editorial Coordinator, Clinical Cardiology and Cardiovascular Interventions, Auctores Publishing LLC. I appreciate the journal (JCCI) editorial office support, the entire team leads were always ready to help, not only on technical front but also on thorough process. Also, I should thank dear reviewers’ attention to detail and creative approach to teach me and bring new insights by their comments. Surely, more discussions and introduction of other hemodynamic devices would provide better prevention and management of shock states. Your efforts and dedication in presenting educational materials in this journal are commendable. Best wishes from, Farahnaz Fallahian.
Dear Maria Emerson, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews, Auctores Publishing LLC. I am delighted to have published our manuscript, "Acute Colonic Pseudo-Obstruction (ACPO): A rare but serious complication following caesarean section." I want to thank the editorial team, especially Maria Emerson, for their prompt review of the manuscript, quick responses to queries, and overall support. Yours sincerely Dr. Victor Olagundoye.

Dear Ashley Rosa, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews. Many thanks for publishing this manuscript after I lost confidence the editors were most helpful, more than other journals Best wishes from, Susan Anne Smith, PhD. Australian Breastfeeding Association.

Dear Agrippa Hilda, Editorial Coordinator, Journal of Neuroscience and Neurological Surgery. The entire process including article submission, review, revision, and publication was extremely easy. The journal editor was prompt and helpful, and the reviewers contributed to the quality of the paper. Thank you so much! Eric Nussbaum, MD
Dr Hala Al Shaikh This is to acknowledge that the peer review process for the article ’ A Novel Gnrh1 Gene Mutation in Four Omani Male Siblings, Presentation and Management ’ sent to the International Journal of Clinical Case Reports and Reviews was quick and smooth. The editorial office was prompt with easy communication.

Dear Erin Aust, Editorial Coordinator, Journal of General Medicine and Clinical Practice. We are pleased to share our experience with the “Journal of General Medicine and Clinical Practice”, following the successful publication of our article. The peer review process was thorough and constructive, helping to improve the clarity and quality of the manuscript. We are especially thankful to Ms. Erin Aust, the Editorial Coordinator, for her prompt communication and continuous support throughout the process. Her professionalism ensured a smooth and efficient publication experience. The journal upholds high editorial standards, and we highly recommend it to fellow researchers seeking a credible platform for their work. Best wishes By, Dr. Rakhi Mishra.

Dear Jessica Magne, Editorial Coordinator, Clinical Cardiology and Cardiovascular Interventions, Auctores Publishing LLC. The peer review process of the journal of Clinical Cardiology and Cardiovascular Interventions was excellent and fast, as was the support of the editorial office and the quality of the journal. Kind regards Walter F. Riesen Prof. Dr. Dr. h.c. Walter F. Riesen.

Dear Ashley Rosa, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews, Auctores Publishing LLC. Thank you for publishing our article, Exploring Clozapine's Efficacy in Managing Aggression: A Multiple Single-Case Study in Forensic Psychiatry in the international journal of clinical case reports and reviews. We found the peer review process very professional and efficient. The comments were constructive, and the whole process was efficient. On behalf of the co-authors, I would like to thank you for publishing this article. With regards, Dr. Jelle R. Lettinga.

Dear Clarissa Eric, Editorial Coordinator, Journal of Clinical Case Reports and Studies, I would like to express my deep admiration for the exceptional professionalism demonstrated by your journal. I am thoroughly impressed by the speed of the editorial process, the substantive and insightful reviews, and the meticulous preparation of the manuscript for publication. Additionally, I greatly appreciate the courteous and immediate responses from your editorial office to all my inquiries. Best Regards, Dariusz Ziora

Dear Chrystine Mejia, Editorial Coordinator, Journal of Neurodegeneration and Neurorehabilitation, Auctores Publishing LLC, We would like to thank the editorial team for the smooth and high-quality communication leading up to the publication of our article in the Journal of Neurodegeneration and Neurorehabilitation. The reviewers have extensive knowledge in the field, and their relevant questions helped to add value to our publication. Kind regards, Dr. Ravi Shrivastava.
Dear Clarissa Eric, Editorial Coordinator, Journal of Clinical Case Reports and Studies, Auctores Publishing LLC, USA Office: +1-(302)-520-2644. I would like to express my sincere appreciation for the efficient and professional handling of my case report by the ‘Journal of Clinical Case Reports and Studies’. The peer review process was not only fast but also highly constructive—the reviewers’ comments were clear, relevant, and greatly helped me improve the quality and clarity of my manuscript. I also received excellent support from the editorial office throughout the process. Communication was smooth and timely, and I felt well guided at every stage, from submission to publication. The overall quality and rigor of the journal are truly commendable. I am pleased to have published my work with Journal of Clinical Case Reports and Studies, and I look forward to future opportunities for collaboration. Sincerely, Aline Tollet, UCLouvain.

Dear Ms. Mayra Duenas, Editorial Coordinator, International Journal of Clinical Case Reports and Reviews. “The International Journal of Clinical Case Reports and Reviews represented the “ideal house” to share with the research community a first experience with the use of the Simeox device for speech rehabilitation. High scientific reputation and attractive website communication were first determinants for the selection of this Journal, and the following submission process exceeded expectations: fast but highly professional peer review, great support by the editorial office, elegant graphic layout. Exactly what a dynamic research team - also composed by allied professionals - needs!" From, Chiara Beccaluva, PT - Italy.

Dear Maria Emerson, Editorial Coordinator, we have deeply appreciated the professionalism demonstrated by the International Journal of Clinical Case Reports and Reviews. The reviewers have extensive knowledge of our field and have been very efficient and fast in supporting the process. I am really looking forward to further collaboration. Thanks. Best regards, Dr. Claudio Ligresti
Dear Chrystine Mejia, Editorial Coordinator, Journal of Neurodegeneration and Neurorehabilitation. “The peer review process was efficient and constructive, and the editorial office provided excellent communication and support throughout. The journal ensures scientific rigor and high editorial standards, while also offering a smooth and timely publication process. We sincerely appreciate the work of the editorial team in facilitating the dissemination of innovative approaches such as the Bonori Method.” Best regards, Dr. Giselle Pentón-Rol.
