AUCTORES
Globalize your Research
Research Article | DOI: https://doi.org/10.31579/2641-0419/076
1Department of Medicine, Institute of Clinical Sciences in Lund, Lund University, Sweden.
2Department of Emergency and Internal medicine, Lund University Hospital of Skåne, Sweden.
*Corresponding Author: Isak Lindstedt, Department of Medicine Institute of Clinical Sciences in Lund Lund University, S22185 Lund, Sweden, Phone: + 46 734 386425
Citation: Lindstedt I., Edvinsson L., Marie-L. Edvinsson., (2020) High Dose Loop-Diuretic Treatment Results in Higher Mortality Rate in Elderly Heart Failure Patients (>80 years) versus Standardized Neuroendocrine Treatment. J. Clinical Cardiology and Cardiovascular Interventions, 3(8);Doi:10.31579/2641-0419/076
Copyright: © 2020 Isak Lindstedt, This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 13 August 2020 | Accepted: 24 August 2020 | Published: 01 September 2020
Keywords: loop-diuretic; mortality; heart failure; neuroendocrine
Introduction
Most chronic heart failure (HF) patients receive therapy with non-potassium-sparing diuretics (loop diuretics), which are fundamental drugs used to prevent multi-organ failure and improve symptoms. The use of diuretics in HF is also associated with neuroendocrine activation, organ damage and increased mortality. However, there is a lack of studies in the very elderly over the age of eighty.
Methods
The study included 99 elderly patients with HF, mean age 81 years, which represented a cohort of patients gathered during recent years. They had been admitted to the internal medicine ward at Lund University Hospital and had been given the primary diagnosis of HF. The patients were divided into two groups based upon the dose of furosemide they had at discharge. Patients receiving less than 80 mg daily were allocated to the low-dose furosemide group (LD-group), 65 patients, and patients receiving 80 mg or more of furosemide, 34 patients, were allocated to the high-dose furosemide group (HD-group).
Results
The HD-group received a mean of 118 mg/day of furosemide and the LD-group received a mean of 39 mg/day of furosemide (p < 0.01). The main finding was that the HD-group had an increased 6 month mortality compared to the LD-group (p = 0.03). Also, both groups demonstrated significant decreases in mean NT-proBNP values from enrollment into the hospital compared to follow up (p < 0.01).
Conclusions
Elderly patients (>80 years of age) were enrolled into the hospital with the diagnosis of severe HF. During treatment they showed higher 6-month mortality when therapy was focused on high doses of furosemide as compared to low doses combined with neuroendocrine therapy. The use of non-potassium-sparing diuretics in the elderly is not unproblematic and this group of patients respond favourable to neuroendocrine treatment.
The prevalence of heart failure (HF) is approximately 1–2% of the adult population in developed countries, but over 10 % among people 70 years of age. The cause of HF is usually a myocardial abnormality. However, defects of the valves, pericardium, endocardium, heart rhythm and conduction can also be involved and more than one abnormality is often present [1]. Systolic and/or diastolic ventriculardysfunction and fluid overload are the main manifestations of HF. The pathophysiological cornerstones of HF are neurohormonal/neuroendocrine activation via the renin-angiotensin-aldosterone system and the sympathetic nervous system. The heart is also somewhat of an endocrine organ that releases natriuretic peptides, like NT-proBNP, that are possible to measure in the blood. [1,2] Furthermore, it is well established that HF is a disorder associated with severe adverse outcomes and a poor prognosis.[3] Most chronic HF patients receive therapy with non-potassium-sparing diuretics. [4] These loop diuretics are the fundamental drugs used to prevent multi-organ failure and improve symptoms in these patients. [5] However, Use of diuretics in HF is associated with further activation of neuroendocrine systems. [6] Diuretics can cause disease progression by increasing myocardial fibrosis [7,8] and worsen renal function [9]. Risks and benefits of loop diuretics have been reevaluated and questioned, particularly the dosage and administration procedure [10]. Several observational studies have shown that static drug exposure is associated with adverse outcomes. In trials examining the use of loop diuretics compared to the non-use of the same, the use of loop diuretics have been associated with poor outcomes such as increased death and rehospitalizations [11-14], For example, in one study on 1302 propensity-matched patients with a mean age of 71 years of age, all-cause mortality occurred in 173 patients not receiving diuretics and 208 patients receiving diuretics, hazard ratio (HR) = 1.36 (Confidence interval (CI) = 1.08-1.71)[13]. Also, in trails comparing the dose of the diuretic, high dose regimens have been associated with increased adverse outcomes compared to low dose regimens [15,18]. Furthermore, the use of potassium-sparing diuretics in patients with HF has been associated with a reduced risk of death compared to the use of non-potassium-sparing diuretics in such patients [19]. Even though the association between loop diuretics and outcome have been demonstrated in several observational studies, some have shown conflicting results [20-22]. There is the argument that the association is merely a marker of disease severity than the cause of it [16]. Most importantly, there is still a lack of studies among the very elderly HF patients over the age of eighty. We hypothesized that elderly HF patients, often frail and with many organs affected, receiving higher doses of furosemide would have a worse outcome than elderly HF patients receiving lower doses of furosemide in combination with neuroendocrine therapy.
Methods
The 99 patients with HF represented a cohort of patients gathered during recent years. They had been admitted to the internal medicine ward at Lund University Hospital and had been given the primary diagnosis of HF. The inclusion criteria was that NT-proBNP tests and blood pressure tests had to been taken at least twice during the hospital stay. The HF patients were divided into two groups based upon the dose of furosemide they had at discharge. Patients receiving less than 80 mg were allocated to the low-dose furosemide group, 65 patients, and patients receiving 80 mg or more, 34 patients, were allocated to the high-dose furosemide group. The cut-off dosage was not established arbitrarily, but was based on the information from previous studies [11,16]. In these trials meaningful comparisons were possible at this cut-off level with the power to detect a difference. We attained relevant information about the patients from their medical records. We obtained basic demographic information about age, gender, BMI, pulse, blood pressure, physical finds and laboratory data at admission. We recorded types of drugs and diagnoses at discharge, total number of drugs at discharge, and number of deaths within 6 months. Six month all-cause mortality was confirmed by reviewing the patients’ medical records and confirming which patients were alive and which were not 6 month after discharge from the hospital, also checking with the Swedish National Death Registry when needed.
Calculations for comparison between the two groups were done using the Student’s T-test for continuous variables and the Pearson’s Chi-square test for dichotomous variables. Paired Samples T-test was used when comparing in-group differences between two values. Statistical significance was set at p < 0.05. Statistics were performed using the IBM SPSS Statistics 25 program.
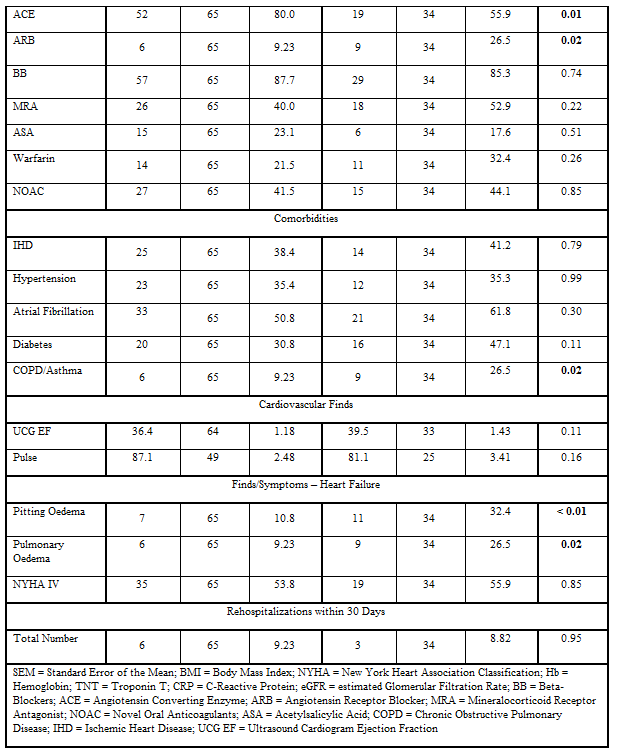
The final results can be seen in (Table 1, 2 and 3, and Figure 1. Table 1) shows basic demographic parameters. The two groups had the same mean age and gender distribution, but the HD-group had a higher BMI. Overall, the standard laboratory tests were similar in the two groups. In addition, the two groups had the same drug treatment when it came to anticoagulant therapy, mineralocorticoid antagonist therapy and beta-adrenoceptor blocker treatment. However, the HD-group had a higher mean number of total drugs and also had somewhat more treatment with angiotensin receptor blockers. On the other hand, the LD-group were treated to a greater extent with the standard of care medications for HF with neuroendocrine therapy, e.g. angiotensin converting enzyme inhibitors. The two groups had similar comorbidities, even though the HD-group had somewhat more chronic obstructive pulmonary disease and asthma. The HD-group had more physical signs of decompensation in the form of pulmonary and peripheral edema, yet the number of HF patients in NYHA IV were the same between the groups. The number of rehospitalizations within 30 days were also the same.
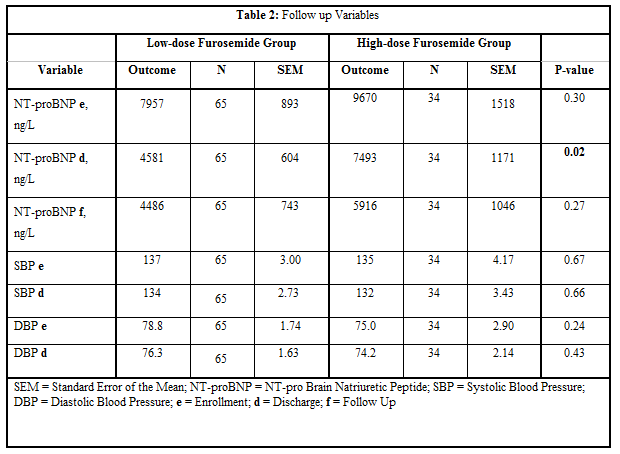
Table 2 presents the results of tests that were performed repeatedly. The mean NT-proBNP value at discharge from the hospital was significantly lower in the LD-group compared to the HD-group. Otherwise, the mean NT-proBNP values and blood pressure values were similar at the given time points.
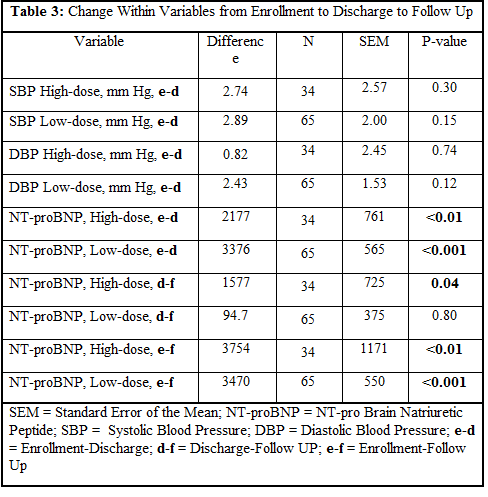
Table 3 depicts the change within variables from enrollment to discharge, from discharge to follow up, and from enrollment to follow up within each study group. Even though the blood pressure values decreased from enrollment to discharge, there was not seen any significant difference in either study group. Overall, there were statistically significant decreases in NT-proBNP values from enrollment to discharge and from enrollment to follow up in both study groups.
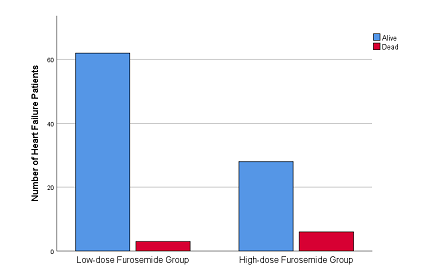
In this study we had elderly patients with severe HF that received somewhat different modes of therapy; the HD-group received a mean dose of 118 mg/day of furosemide at discharge from the hospital and had higher 6 months mortality than patients from the LD-group that received a mean dose of 39 mg/day of furosemide, but were usually combined with neuroendocrine therapy. The results are important because this association between diuretic dose and mortality has not been studied extensively in patients over the age of 80. To the best of our knowledge, most studies up to date have included patients with a mean age between 50 and 79 years of age. This is central because it might be that the difference in mortality between low dose therapy and high dose therapy of loop diuretics is even more pronounced in the elderly population; patients who have more severe heart failure, greater tendency to congestion, numerous concomitant diseases, and are prone to side effects and interactions between drugs. For example, the trials and their respective study arms referenced to in this paper, had the following age demographics: mean age of 53 and 56 years [15]; mean age of 55 and 58 years [18]; mean age of 53 and 60 years [16]; mean age of 59, 61, 61, and 62 years [19]; mean age of 62.6 and 62.9 years [12]; mean age of 67, 69, and 72 years [11]; mean age of 69.8 and 70.9 years [14]; mean age of 71.5 and 71.6 years [13]; and, finally, mean age of 77.3, 78.4 and 78.7 years [17]. We had a mean age of 80.9 and 81.8 years.
The ways furosemide interacts with the cardiovascular system are still worth studying and the exact pathophysiological pathways through which it determines the prognosis of HF remain poorly investigated and understood. [18] Nonetheless, there are several probable pathophysiological effects of furosemide that could harm the human body. Furosemide acts on the Na+-K+-2Cl−cotransporter in the thick ascending limb of the loop of Henle. Its main function is to inhibit sodium and chloride reabsorption [23]. Frequently observed adverse drug reactions to furosemide is hypokalemia and/or hypomagnesemia[24]. These abnormalities could lead to potentially deleterious arrhythmogenic effects in elderly patients with chronic HF. [25] Furthermore, furosemide causes intravascular volume depletion. A decreased intravascular volume could lead to hypotension with the risk of orthostatic hypotension which is associated with increased mortality in elderly HF patients. [26] Also, intravascular volume depletion can cause a reduced glomerular filtration rate and renal dysfunction. It is well known that renal dysfunction predicts mortality in hospitalized patients with HF. [27]
There was a significant difference in mean creatinine values at baseline between the LD-group and the HD-group in our study (Table 1). However, there was no significant difference in eGFR nor in the number of HF patients with renal failure (data not shown) at baseline. Whether the increased 6 month mortality that we saw was a consequence of increased renal failure caused by higher doses of furosemide, or was merely a marker of greater sickness in the HD-group because of habitual renal failure independent of furosemide treatment, is unclear. In a similar line of thought, congestion seemed to be greater in the HD-group since they presented with significantly more symptomatic disease such as pulmonary and peripheral edema. Yet, the number of HF patients in NYHA IV, mean left ventricular ejection fraction, and mean NT-proBNP values at admittance were similar between the groups. It appears logical that the HF patients in the HD-group were treated with higher doses of furosemide by their general physician before hospitalization and/or by the hospital physician when confronted with more physical signs of HF. But we might speculate that this action also could be the very reason behind the higher mortality in the HD-group. Higher doses of furosemide might very well help alleviating the immediate symptoms of HF, but over time lead to diuretic resistance, electrolyte disturbances, intravascular volume depletion, renal dysfunction and death. On the other hand, there is still the possibility that the greater congestion seen in the HD-group was a sign of greater HF disease (and renal disease because of increased creatinine levels) in this group compared to the LD-group finally leading to greater death. [28]
There are many common causes of diuretic resistance such as incorrect diagnosis of the disease, nonadherence to recommended sodium and/or fluid restriction, nonadherence to the drug, the dose of the drug is too low or infrequent, or absorption of the drug is poor. [29] Furthermore, there are many renal issues involved in diuretic resistance best divided into reduced diuretic secretion or insufficient kidney response to the drug. Decreased kidney blood flow and/or decreased functional kidney mass hinders secretion and low glomerular filtration rate and/or activation of the renin-angiotensin system hampers the kidneys response to the drug. [29] The increased congestion in the HD-group could have contributed to the diuretic resistance by limiting absorption of furosemide e.g. because of mucosal edema of the intestine, decreased intestinal perfusion and reduced intestinal motility. [30] Indeed, there are many pharmacokinetic and pharmacodynamic considerations to take into account when evaluating loop diuretics in disease states such as HF and renal failure. [31]
Increased levels of NT-proBNP have been associated with increased mortality in HF patients [32] and, along the same lines, reductions in NT-proBNP have been associated with improved outcomes. [33] Considering this fact, we might have expected that meaningful decreases in NT-proBNP levels from admittance, through discharge from the hospital, to follow up would improve survival of the patients in the two groups. Both groups showed significant reductions in mean values of NT-proBNP from enrollment to follow up. Yet, there were more deaths in the HD-group than the LD-group. Interestingly, the reduction of the mean NT-proBNP value from discharge to follow up in the HD-group was significant, 1577 ng/L (p=0.04), while the reduction of the mean NT-proBNP value during the same time frame in the LD-group was meager, 94.7 ng/L (p=0.80). A substantial reduction in natriuretic peptides in the HD-group still led to increased mortality. This finding is novel and important since it suggests that the potential harmful effects of high dose furosemide overrides the known beneficial effects of decreasing natriuretic peptides. The use of therapy mainly focused on administration of high doses of loop diuretics with early diuretic effect (but in our patients this did not show up as reduction in body weight). The LD-group had the same entry conditions and there was no difference between the groups in NT-proBNP, neither at enrollment nor at follow-up (Table 2). However, the mortality rate was significantly higher in the HD-group versus the LD-group of diuretic based therapy (Figure 1). The reason might rely on the positive effect offered by treating the sympathetic over activity with a beta-adrenoceptor blocker, antagonizing the over activity of the renin-angiotensin-aldosterone pathway. The caveat is that neuroendocrine therapy works equally well in the elderly as in younger patients.
We have recently shown that elderly patients (84.6 years of age) with HF treated with intravenous bolus injections of furosemide had lower mortality than elderly heart failure patients (80.1 years of age) treated with continuous intravenous infusions of furosemide. [34] One logical reasons for this could be less persistent kidney damage caused by the diuretic when it was given intermittently, which also might have led to less neuroendocrine overdrive. On the contrary, in a randomized controlled trial in HF patients with acute decompensation and high risk of diuretic resistance, continuous infusion of furosemide was associated with better decongestion than intermittent bolus of furosemide [35]. Also, in the largest prospective randomized trial comparing the two modes of administration of furosemide in acute decompensated HF, the DOSE study, no significant differences were found between bolus and continuous therapy. [36] However, the patients included in both these trials were significantly younger than in our study, mean age about 60 and 66 years of age respectively, making a comparison more difficult. In the current study we showed that a low dose regimen of furosemide was superior to a high dose regimen in eighty year olds, putatively because of less diuretic resistance and less potential harmful pathophysiological effects. Based on these observations, we suggest that it might be more appropriate to treat HF patients in their eighties with intermittent and low doses of diuretics in order to improve outcome. In favor of this argument, a recent study have shown that diuretic withdrawal in stable outpatients with mild heart failure did not increase self-perception of dyspnea, the need for reuse of furosemide and heart failure related events were infrequent [37].
Limitations and future directions: This is a relatively small study and to the best of our knowledge the first study that has solely examined patients in their eighties. Larger studies in even older patients might give further insight. A randomized controlled trial would be optimal, but is not possible to undertake since HF patients are treated based on their need of symptom relief which may differ from patient to patient. Also, it would seem unethical to withhold diuretics for patients in need or add diuretics to patients that do not require them. We have shown that it is possible to improve the outcome of HF patients by standardizing the care of these patients when they are admitted to the hospital with increased congestive symptoms [38]. We now propose that a new improved standardized plan might be implemented based on intermittent and low dose diuretic treatment in acute HF.
Conclusions: We advocate careful use of loop diuretics, only to improve symptoms in the very elderly patients (>80 years), and to be used in a balanced way with neuroendocrine therapy modes. With angiotensin converting enzyme inhibitors, angiotensin receptor blockers, mineralocorticoid receptor antagonist, and beta-adrenoceptor blockers in well titrated doses the circulation to vital organs such as the brain, the heart and the kidneys is maintained.