AUCTORES
Globalize your Research
Research Article | DOI: https://doi.org/10.31579/2578-8965/214
1Department of Obstetrics and Gynaecology, Abia State University, Uturu, Nigeria
2Department of Surgery, Abia State University, Uturu, Nigeria
3Department of Haematology and Blood Transfusion, University of Port Harcourt, Rivers State, Nigeria
4Department of Biochemistry, Federal University of Technology, Owerri, Imo State, Nigeria
*Corresponding Author: A. I. Airaodion, Department of Biochemistry, Federal University of Technology, Owerri, Imo State, Nigeria.
Citation: E. O. Ezirim, E. M. Akwuruoha, C. O. Onyemereze, I. O. Abali, A. I. Airaodion, et al. (2024), Evaluation of Antithrombin-III Activity and Platelet Count in Pregnancy-Induced Hypertension among Pregnant Women attending Antenatal care in a Tertiary Health Facility in Southeast, Nigeria, J. Obstetrics Gynecology and Reproductive Sciences, 8(3) DOI:10.31579/2578-8965/214
Copyright: © 2024, A. I. Airaodion. This is an open-access article distributed under the terms of The Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 05 April 2024 | Accepted: 15 April 2024 | Published: 24 April 2024
Keywords: antenatal care; antithrombin-iii; platelet count; preeclampsia; pregnancy-induced hypertension
Background: Pregnancy-induced hypertension (PIH) is a significant health issue that affects maternal and fetal outcomes. Antithrombin-III (AT-III) and platelet count alterations could serve as pivotal indicators for the management and prognosis of PIH.
Objective: This study aimed to assess AT-III activity and platelet counts in pregnant women with and without PIH at the Federal Medical Centre (FMC), Owerri, Imo State, Nigeria.
Methods: A case-control cross-sectional analytical study design was employed, including 135 pregnant women with PIH and 135 age-matched normotensive pregnant women. Exclusion criteria comprised chronic hypertension, known thrombophilic disorders, or anticoagulant therapy before pregnancy. AT-III levels and platelet counts were compared between groups using SPSS version 20.0, with significance set at p ≤ 0.05.
Results: AT-III activity was significantly lower in the PIH group (75.45±6.23%) compared to the normotensive group (96.84±9.64%, p=0.028). Similarly, platelet count was significantly reduced in the PIH group (170.90 ±8.78 x109/L) versus the normotensive group (191.56±6.54 x109/L, p=0.032). No significant differences were found in sociodemographic variables except for the trimester of antenatal care registration and history of preeclampsia in previous pregnancies.
Conclusion: This study highlights significant reductions in AT-III activity and platelet count among pregnant women with PIH, suggesting these parameters' potential role in PIH management and prognosis. These findings emphasize the importance of monitoring AT-III levels and platelet count as part of the antenatal care protocol in pregnant women, particularly those with or at risk for PIH.
Pregnancy-Induced Hypertension (PIH), also known as preeclampsia, is a complex hypertensive disorder affecting 2-8% of pregnancies worldwide and remains a leading cause of maternal and perinatal morbidity and mortality [1]. Characterized by high blood pressure and signs of damage to another organ system, most often the liver and kidneys, after 20 weeks of gestation in a woman previously diagnosed with normal blood pressure [2]. The pathophysiology of preeclampsia is not entirely understood, but it is believed to involve abnormal placental development leading to placental ischemia, oxidative stress, and endothelial dysfunction [3].
Antithrombin-III (AT-III) is a critical protein in the coagulation pathway, acting as a natural anticoagulant that helps regulate blood clot formation. Reduced AT-III levels have been associated with an increased risk of thrombosis and have been observed in various pregnancy complications, including preeclampsia [4].
Platelets play a crucial role in hemostasis, and thrombocytopenia (a low platelet count) is a common feature in preeclampsia, contributing to its complications [5]. Investigating the association between AT-III levels, platelet count, and preeclampsia can provide insights into the disease's pathophysiology and potential therapeutic targets.
The prevalence of PIH varies by geographical location, due to differences in genetic, environmental, and socio-economic factors. In Nigeria, and particularly in the Southeast region, the prevalence of PIH has been reported to be higher than in some other parts of the world. This variation can be attributed to factors such as dietary habits, access to healthcare, and awareness of PIH among pregnant women [6].
In Southeast Nigeria, antenatal care services play a crucial role in the early detection and management of PIH. However, there are challenges such as limited resources, inadequate healthcare infrastructure, and low patient literacy levels that may affect the effective monitoring and management of this condition [7].
Given the significant impact of PIH on maternal and fetal health, and the potential role of AT-III and platelet count in predicting and managing this condition, there is a need for more focused research in high-prevalence areas like Southeast Nigeria. Understanding the dynamics of AT-III activity and platelet count among pregnant women with PIH attending antenatal care in this region can provide insights necessary for developing targeted interventions to improve pregnancy outcomes.
Study Design
This is a case-control cross-sectional analytical study aimed to evaluate the association between Antithrombin-III levels and platelet count in pregnant women with and without pregnancy-induced hypertension (PIH) attending antenatal care at the Federal Medical Centre (FMC), Owerri, Imo State, Nigeria.
Inclusion Criteria: Pregnant women attending antenatal care at the teaching hospital, both with diagnosed pregnancy-induced hypertension (preeclampsia) and normotensive pregnant women as controls.
Exclusion Criteria: Women with chronic hypertension, known thrombophilic disorders, or on anticoagulant therapy prior to pregnancy.
Sample Size Determination
The sample size was determined based on the expected difference in Antithrombin-III levels and platelet counts between the two groups, considering the prevalence of preeclampsia in Nigeria.
It was determined using the Fisher’s formula outlined by Ekeleme et al. [8]:
n = (Z^2 (Pq))/e^2
where n = minimum sample size
Z = 1.96 at 95% confidence level,
P = known prevalence of preeclampsia in Nigeria
e = error margin tolerated at 5% = 0.05
q = 1 - p
According to Musa et al. [9], the prevalence of preeclampsia in Nigeria is 8.8%.
P = 8.8% = 0.088
q = 1 – p
= 1 – 0.088
= 0.912
n = ((1.96) ^2 (0.088 x 0.912))/〖 (0.05) 〗^2
n = (0.3083114496)/ (0.0025) = 123.32
The minimum sample size was 123 and was adjusted to 135 to account for non-response rate of 10 %.
Sampling Technique
Stratified random sampling was utilized for this study, with the strata being women with PIH and those without. Women were randomly selected from each stratum to participate in the study. Thus, one hundred and thirty-five (135) pregnant women with PIH and one hundred and thirty-five (135) age-matched normotensive pregnant women were recruited for the study.
Data Collection Methods
A structured questionnaire was utilized to collect the data. The questionnaire was composed of three sections: (1) Sociodemographic Details of Participants, (2) Obstetric History of Participants (3) Medical and Lifestyle Information of Participants. The questionnaire was developed and validated through extensive literature review and expert opinion, ensuring that it covered all pertinent information required for the study.
Determination of Anthropometric Indices and Blood Pressure
The body mass index for each participant was calculated from weight and height measurements obtained through the use of Hanson’s weighing scale (capacity of 120 kg) and a meter rule attached to a wooden pole, respectively as described by Agu et al. [10]. Briefly, the participants were weighed in light clothing and reading was taken to the nearest 0.1 kg. Height to the nearest 0.1 cm was measured with the participants standing erect on a flat surface. Waist circumference was measured with a flexible non-stretch tape placed on the midpoint between the top of the iliac crest and the bottom of the rib cage where the last palpable rib is found [10]. The weighing scale was maintained at zero before taking the weight measurements.
Blood pressure was determined twice (a minimum of 3 mins interval was observed) by trained research assistants using Omron automatic sphygmomanometer (M2: HEM-7121-E, Vietnam) with the participant sitting comfortably and arm resting on a table at the same level with the heart as described by Ijioma et al. [11]. Average of the two readings was used in the analysis. Preeclampsia was diagnosed according to American college of Obstetrics and Gynaecology (ACOG) criteria [1]: a blood pressure higher than 140/90 mm Hg and proteinuria more than 300mg/24hr were observed on at least two occasions more than 6 hours apart after the 20th weeks of pregnancy.
Determination of Platelet Counts and AT-III
For platelet counts, blood samples were collected in EDTA tubes and plasma was separated after centrifugation for 5-10 minutes at 3000 rpm within one hour of the venepuncture. Haematological parameter (platelet counts) was performed on cell counter PCN-201(N) according to the method described by Chikezie et al. [12]. For Coagulation parameter (AT-III), blood was placed into test tubes containing 1 ml of 3.8% sodium-citrate. Centrifugation of these specimens was done for ten minutes at room temperature and at 2500˟ g. The level of AT-III was studied using the fully automatic Coagulometer equipment (Diagnostic Stago STA Compact; France).
Supervision and technical support were provided to trained research assistants throughout the study period to ensure study protocols were followed as planned. On the spot random checks of collected data were conducted and identified inconsistencies/missing data were fixed. Weight and blood pressure equipment were checked after each measurement to ensure continued functionality.
Data Analysis
The statistical package for the social science (SPSS) was used to analyze the collected data (version 20.0; SPSS, Chicago, IL). The mean, standard deviation and t-test were the statistical tests employed in this investigation. Simple tables containing frequencies, percentages, and mean values were used to display the obtained results. The threshold of statistical significance for group comparisons was set at P-value ≤ 0.05.
Ethical Consideration
The research was conducted in accordance with ethical principles, including informed consent, confidentiality, and data protection. Participants were informed of the purpose of the research and had the option to withdraw at any time without any consequences.
In terms of sociodemographic details (Table 1), the age distribution among hypertensive and normotensive subjects did not show significant differences, with the majority being in the 30-39 age range for both groups (58.52% vs. 59.26%, p=0.494). Educational levels and marital status also did not significantly differ between the groups, with the largest proportion having secondary education (38.52% hypertensive vs. 52.59% normotensive, p=0.175) and being married (57.78% hypertensive vs. 86.67% normotensive, p=0.121).
Obstetric history (Table 2) revealed that gravidity and parity were not significantly different between the two groups. However, the timing of antenatal care registration and the history of preeclampsia showed significant differences. A smaller proportion of hypertensive women registered for antenatal care in the first trimester compared to normotensive subjects (14.81% vs. 25.19%, p=0.046), and a higher proportion of hypertensive women had a history of preeclampsia (46.67% vs. 16.30%, p=0.027).
Medical and lifestyle information (Table 3) indicated significant differences in previous diagnoses of hypertension or preeclampsia, family history of these conditions, smoking history, alcohol consumption, complications in previous pregnancies, pre-existing medical conditions, and physical activity levels. Notably, a higher proportion of hypertensive patients had a previous diagnosis (57.78% vs. 28.89%, p=0.009), a family history (60.00% vs. 32.59%, p=0.014), and reported experiencing complications in previous pregnancies (33.33% vs. 18.52%, p=0.004). Additionally, hypertensive patients were more likely to lead a sedentary lifestyle (61.48% vs. 26.67%, p=0.033).
Anthropometric parameters (Table 4) showed no significant difference in mean body mass index (BMI) or waist-hip ratio between the two groups. However, mean systolic and diastolic blood pressures were significantly higher in hypertensive patients (141.76 mmHg vs. 116.53 mmHg, p=0.007 for systolic; 98.43 mmHg vs. 76.82 mmHg, p=0.003 for diastolic).
Laboratory measures (Figures 1 and 2) revealed that hypertensive patients had significantly lower antithrombin-III activity (75.45% vs. 96.84%, p=0.028) and platelet count (170.90 x109/L vs. 191.56 x109/L, p=0.032) compared to normotensive subjects, indicating altered coagulation status.
| Variable | Hypertensive Patients n (%) | Normotensive Subjects n (%) | p-value |
| Age (in Years) | 0.494 | ||
| Less than 20 | 3 (2.22) | 6 (4.44) | |
| 20 – 29 | 22 (16.30) | 20 (14.81) | |
| 30 – 39 | 79 (58.52) | 80 (59.26) | |
| 40 and above | 31 (22.96) | 29 (21.48) | |
| Educational Level | 0.175 | ||
| No formal Education | 21 (15.56) | 11 (8.15) | |
| Primary Education | 32 (23.70) | 21 (15.56) | |
| Secondary Education | 52 (38.52) | 71 (52.59) | |
| Tertiary Education | 30 (22.22) | 32 (23.70) | |
| Marital Status | 0.121 | ||
| Single | 39 (28.89) | 7 (5.19) | |
| Married | 78 (57.78) | 117 (86.67) | |
| Divorced/Widowed | 18 (13.33) | 11 (8.15) |
Table 1: Sociodemographic Details of Participants
p-value  0.05 are statistically significant
0.05 are statistically significant
| Variable | Hypertensive Patients n (%) | Normotensive Subjects n (%) | p-value |
| Gravidity (Number of pregnancies, including the current one) | 0.082 | ||
| 1 | 40 (29.63) | 55 (40.74) | |
| 2 | 48 (35.56) | 46 (34.07) | |
| 3 | 27 (20.00) | 15 (11.11) | |
| 4 | 11 (8.15) | 13 (9.63) | |
| More than 4 | 9 (6.67) | 6 (4.44) | |
| Parity (Number of births after 28 weeks of gestation) | 0.128 | ||
| 0 | 48 (35.56) | 55 (40.74) | |
| 1 | 51 (37.78) | 46 (34.07) | |
| 2 | 23 (17.04) | 21 (15.56) | |
| 3 | 8 (5.93) | 10 (7.41) | |
| 4 | 3 (2.22) | 2 (1.48) | |
| More than 4 | 2 (1.48) | 1 (0.74) | |
| What trimester did you register for antenatal care? | 0.046* | ||
| First Trimester | 20 (14.81) | 34 (25.19) | |
| Second Trimester | 104 (77.04) | 89 (65.93) | |
| Third Trimester | 11 (8.15) | 12 (8.89) | |
| History of Preeclampsia in Previous Pregnancies | 0.027* | ||
| Yes | 63 (46.67) | 22 (16.30) | |
| Not | 32 (23.70) | 58 (42.96) | |
| Not Applicable | 40 (29.63) | 55 (40.74) | |
| *Outcome of Previous Pregnancies (Check all that apply) | 0.092 | ||
| Live birth | 82 (56.16) | 70 (50.36) | |
| Stillbirth | 7 (4.79) | 3 (2.16) | |
| Miscarriage | 12 (8.22) | 9 (6.47) | |
| Premature birth | 5 (11.64) | 2 (1.44) | |
| Not Applicable | 40 (27.40) | 55 (39.57) | |
| *Experienced Symptoms during current pregnancy (Check all that apply) | 0.048* | ||
| Swelling (hands/face/leg) | 41 (25.31) | 51 (30.54) | |
| Severe headache | 56 (34.57) | 39 (23.35) | |
| Vision problems (blurriness, light sensitivity) | 4 (2.47) | 00 (0.00) | |
| Upper abdominal pain | 17 (10.49) | 9 (5.39) | |
| None of the above | 44 (27.16) | 68 (40.72) |
Table 2: Obstetric History of Participants
p-value  0.05 are statistically significant
0.05 are statistically significant
* = Multiple Response
| Variable | Hypertensive Patients n (%) | Normotensive Subjects n (%) | p-value |
| Previous Diagnosis of Hypertension or Preeclampsia | 0.009* | ||
| Yes | 78 (57.78) | 39 (28.89) | |
| No | 57 (42.22) | 96 (71.11) | |
| Family History of Hypertension or Preeclampsia | 0.014* | ||
| Yes | 81 (60.00) | 44 (32.59) | |
| No | 54 (40.00) | 91 (67.41) | |
| Smoking History | 0.036* | ||
| Current smoker | 00 (0.00) | 00 (0.00) | |
| Former smoker | 28 (20.74) | 11 (8.15) | |
| Never smoked | 107 (79.26) | 124 (91.85) | |
| Frequency of alcohol consumption | 0.023* | ||
| Never | 78 (57.78) | 104 (77.04) | |
| Stopped alcohol | 38 (28.15) | 24 (17.78) | |
| Occasionally | 19 (14.07) | 7 (5.19) | |
| Regularly | 00 (0.00) | 00 (0.00) | |
| Have you experienced any complications in your previous pregnancies? | 0.004* | ||
| Yes | 45 (33.33) | 25 (18.52) | |
| No | 90 (66.67) | 110 (81.48) | |
| Do you have any pre-existing medical conditions? (e.g., diabetes, kidney disease) | 0.000* | ||
| Yes | 56 (41.48) | 8 (5.93) | |
| No | 79 (58.52) | 127 (94.07) | |
| Describe your daily physical activity level | 0.033* | ||
| Sedentary (little or no exercise) | 83 (61.48) | 36 (26.67) | |
| Lightly active (light exercise/sports 1-3 days/week) | 41 (30.37) | 63 (46.67) | |
| Moderately active (moderate exercise/sports 3-5 days/week) | 11 (8.15) | 36 (26.67) | |
| Very active (hard exercise/sports 6-7 days a week) | 00 (0.00) | 00 (0.00) | |
| Extra active (very hard exercise/sports & physical job or 2x training) | 00 (0.00) | 00 (0.00) |
Table 3: Medical and Lifestyle Information of Participants
p-value  0.05 are statistically significant
0.05 are statistically significant
| Anthropometric Parameters | Hypertensive Patients | Normotensive Subjects | p-value |
| Mean Body Mass Index (BMI) (kg/m2) | 23.38  4.23 4.23 | 22.97  3.92 3.92 | 0.846 |
| Mean Waist Circumference (cm) | 98.94 7.31 7.31 | 94.03 7.53 7.53 | 0.082 |
| Mean Waist Hip Ratio | 0.95 0.06 0.06 | 0.94 0.04 0.04 | 0.527 |
| Mean Systolic Blood Pressure (mmHg) | 141.76 11.82 11.82 | 116.53 11.31 11.31 | 0.007* |
| Mean Diastolic Blood Pressure (mmHg) | 98.43 11.26 11.26 | 76.82 6.44 6.44 | 0.003* |
Table 4: Anthropometric Parameters of Pregnant Women
p-value  0.05 are statistically significant
0.05 are statistically significant
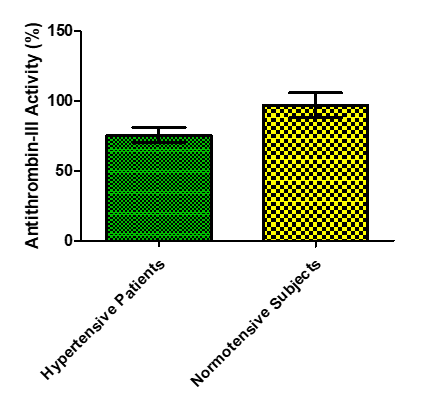
Figure 1: Antithrombin-III Activity of Hypertensive and Normotensive Pregnant Women
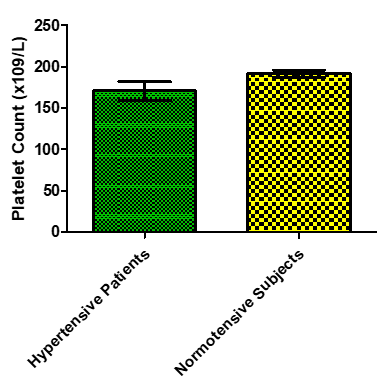
Figure 2: Platelet Count of Hypertensive and Normotensive Pregnant Women
Pregnancy-induced hypertension (PIH) is a significant contributor to maternal and fetal morbidity and mortality, particularly in developing countries. Antithrombin-III (AT-III) activity and platelet count are critical parameters in assessing coagulation status and placental function in pregnant women. This study evaluates the association between AT-III levels and platelet counts in pregnant women with and without PIH attending antenatal care at the Federal Medical Centre (FMC), Owerri, Imo State, Nigeria.
The study observed no significant difference in gravidity and parity between hypertensive and normotensive pregnant women, with p-values of 0.082 and 0.128, respectively. This suggests that the number of pregnancies or births does not significantly influence the likelihood of developing PIH. Previous studies have offered mixed results on this matter. For example, a study by Bartsch, et al. [13] found that higher parity was associated with a reduced risk of preeclampsia, a specific form of PIH, in women with a history of the disease. The discrepancy between these findings may be due to differences in study populations, definitions of hypertension, or the inclusion of various risk factors.
Significantly, more normotensive subjects registered for antenatal care in the first trimester compared to hypertensive patients (p = 0.046). Early antenatal registration may contribute to better monitoring and management of potential hypertensive disorders. This is in line with literature suggesting that early and regular antenatal care can help in early detection and management of preeclampsia and other hypertensive disorders of pregnancy [14].
The study found a significant association between a history of preeclampsia in previous pregnancies and the development of hypertension in the current pregnancy (p = 0.027). This corroborates with previous research indicating that a history of preeclampsia is a strong predictor for recurrence in subsequent pregnancies [15].
Although not statistically significant for the outcome of previous pregnancies, there was a trend towards more adverse outcomes in hypertensive patients. Notably, experienced symptoms during the current pregnancy, such as swelling, severe headache, and vision problems, were more common in hypertensive patients, with a significant difference in vision problems (p = 0.048). This aligns with the known clinical manifestations of PIH and preeclampsia [1].
The study notes a statistically significant difference (p=0.009) between hypertensive patients and normotensive subjects concerning previous diagnoses of hypertension or preeclampsia, with 57.78% of hypertensive patients having a history compared to 28.89% of normotensive subjects. This aligns with findings by Brown et al. [16], who reported that a history of hypertension or preeclampsia increases the risk of PIH in subsequent pregnancies, emphasizing the need for closer monitoring of these patients.
Similarly, a significant difference (p=0.014) was observed in the family history of hypertension or preeclampsia between the two groups, suggesting a genetic predisposition or familial risk factor. This finding is consistent with the literature, which indicates that a family history of these conditions significantly elevates the risk for PIH [17].
The study also found significant differences in the history of smoking and alcohol consumption. Although no current smokers were reported, former smokers constituted a higher percentage in the hypertensive group than in the normotensive group (p=0.036). For alcohol consumption, those who never consumed alcohol were significantly higher in the normotensive group. These results suggest lifestyle modifications as potential interventions for reducing PIH risk. The negative impact of smoking on pregnancy outcomes is well-documented, but its specific role in PIH is complex and multifactorial [18].
A significant correlation was found between complications in previous pregnancies (p=0.004) and pre-existing medical conditions (p=0.000) with PIH. These factors underscore the importance of comprehensive prenatal screening and management of women with such histories to mitigate the risk of PIH.
Physical activity levels showed significant variation, with a sedentary lifestyle being more common among hypertensive patients (p=0.033). This finding suggests that increased physical activity could potentially lower the risk of PIH, supporting the recommendations for moderate exercise during pregnancy [19].
The study reports no significant difference in the mean Body Mass Index (BMI) between hypertensive and normotensive pregnant women, with values of 23.38 ± 4.23 kg/m2 and 22.97 ± 3.92 kg/m2, respectively (p=0.846). This suggests that BMI may not be a distinguishing factor for PIH in this population, aligning with the findings of some studies while contrasting with others that have identified a higher BMI as a risk factor for the development of PIH [20,21]. For instance, Spradley's meta-analysis indicated a correlation between higher pre-pregnancy BMI and an increased risk of developing PIH, suggesting a complex interaction between maternal adiposity and blood pressure regulation during pregnancy.
In terms of waist circumference, the study found a slightly higher mean waist circumference in hypertensive patients (98.94±7.31 cm) compared to normotensive subjects (94.03±7.53 cm), with a p-value of 0.082. Although not statistically significant, this trend towards higher waist circumferences in hypertensive pregnant women could reflect central adiposity's role in PIH pathogenesis. This is supported by evidence suggesting that central obesity may contribute more significantly to cardiovascular risk factors, including hypertension, than total body fat [22].
The waist-hip ratio (WHR), a measure of fat distribution, showed no significant difference between the two groups (0.95±0.06 in hypertensive patients vs. 0.94±0.04 in normotensive subjects; p=0.527). This finding indicates that WHR may not be a critical marker for PIH in this specific population, which could reflect the multifactorial nature of PIH where genetic, environmental, and other metabolic factors play a role beyond simple anthropometric measures.
Significantly, the study found marked differences in mean systolic and diastolic blood pressures between hypertensive and normotensive pregnant women. The hypertensive group had a mean systolic blood pressure of 141.76±11.82 mmHg and a mean diastolic blood pressure of 98.43±11.26 mmHg, significantly higher than the normotensive group (116.53±11.31 mmHg systolic and 76.82±6.44 mmHg diastolic, with p-values of 0.007 and 0.003, respectively). These findings are consistent with the diagnostic criteria for PIH and underscore the condition's impact on cardiovascular strain during pregnancy [23].
The current study's findings on BMI and PIH are consistent with those of Buhimschi et al. [24], who found no significant difference in BMI between women with and without PIH in a cohort study. However, the evidence regarding waist circumference and WHR as predictors of PIH remains mixed. Some studies have suggested that these measures of central adiposity may be more closely linked to metabolic syndromes and cardiovascular disease than to PIH specifically [25].
Regarding blood pressure differences, the results align with the established understanding that PIH is characterized by significantly elevated blood pressure levels. These findings are in line with the broader literature, which consistently shows elevated systolic and diastolic blood pressures in PIH cases [26].
Antithrombin-III, a key anticoagulant, plays a critical role in maintaining hemostatic balance. Its reduced activity in PIH suggests an increased risk of thrombosis, which is a concern given the hypercoagulable state of pregnancy [27]. The observed mean AT-III activity of 75.45±6.23% in hypertensive patients versus 96.84±9.64% in normotensive subjects aligns with earlier studies indicating that AT-III activity decreases as pregnancy progresses and this reduction is more pronounced in women with PIH [28]. For instance, a study by Sharma and colleagues [29] found similar reductions in AT-III levels among women with PIH, reinforcing the association between decreased AT-III activity and the pathogenesis of PIH.
The platelet count findings from the study further illuminate the altered coagulation landscape in PIH. With hypertensive patients showing a mean platelet count of 170.90±8.78 x109/L compared to 191.56±6.54 x109/L in normotensive subjects, there's evidence of thrombocytopenia associated with PIH. This is consistent with the literature, where PIH has been linked to a reduction in platelet count, reflecting increased consumption or destruction of platelets, potentially leading to complications like HELLP syndrome (Hemolysis, Elevated Liver enzymes, and Low Platelet count) [30]. A meta-analysis by Haase et al. [31] corroborated these findings, suggesting that thrombocytopenia could serve as an early marker for PIH diagnosis and severity assessment.
When comparing the current study's findings with previous literature, it is evident that the reduced AT-III activity and platelet count in hypertensive pregnant women are consistent with the broader research narrative. However, the magnitudes of these changes and their clinical implications may vary across populations due to genetic, dietary, and environmental factors. For example, studies in different geographical locations have reported varying degrees of reduction in AT-III activity and platelet count among PIH patients [32], indicating the influence of ethnic and regional differences on the hematological manifestations of PIH.
Reduced AT-III activity and lower platelet counts are associated with pregnancy-induced hypertension, suggesting that these parameters could serve as useful markers in the early detection and management of PIH. The study highlights the importance of comprehensive antenatal care and the potential for targeted interventions to mitigate the risks associated with PIH.
Implications And Future Directions
The findings from this study underscore the importance of monitoring AT-III activity and platelet count in pregnant women, particularly those with or at risk of developing PIH. They suggest that targeted interventions aimed at stabilizing these parameters could mitigate the risk of thrombotic events and improve maternal and fetal outcomes. Future research should explore the underlying mechanisms driving the reduction in AT-III activity and platelet count in PIH, with an eye towards developing predictive models for early identification of women at risk. Additionally, longitudinal studies examining the recovery of these parameters postpartum and their long-term health implications would provide valuable insights into the overall impact of PIH on women's health.
Clearly Auctoresonline and particularly Psychology and Mental Health Care Journal is dedicated to improving health care services for individuals and populations. The editorial boards' ability to efficiently recognize and share the global importance of health literacy with a variety of stakeholders. Auctoresonline publishing platform can be used to facilitate of optimal client-based services and should be added to health care professionals' repertoire of evidence-based health care resources.

Journal of Clinical Cardiology and Cardiovascular Intervention The submission and review process was adequate. However I think that the publication total value should have been enlightened in early fases. Thank you for all.

Journal of Women Health Care and Issues By the present mail, I want to say thank to you and tour colleagues for facilitating my published article. Specially thank you for the peer review process, support from the editorial office. I appreciate positively the quality of your journal.
Journal of Clinical Research and Reports I would be very delighted to submit my testimonial regarding the reviewer board and the editorial office. The reviewer board were accurate and helpful regarding any modifications for my manuscript. And the editorial office were very helpful and supportive in contacting and monitoring with any update and offering help. It was my pleasure to contribute with your promising Journal and I am looking forward for more collaboration.

We would like to thank the Journal of Thoracic Disease and Cardiothoracic Surgery because of the services they provided us for our articles. The peer-review process was done in a very excellent time manner, and the opinions of the reviewers helped us to improve our manuscript further. The editorial office had an outstanding correspondence with us and guided us in many ways. During a hard time of the pandemic that is affecting every one of us tremendously, the editorial office helped us make everything easier for publishing scientific work. Hope for a more scientific relationship with your Journal.

The peer-review process which consisted high quality queries on the paper. I did answer six reviewers’ questions and comments before the paper was accepted. The support from the editorial office is excellent.

Journal of Neuroscience and Neurological Surgery. I had the experience of publishing a research article recently. The whole process was simple from submission to publication. The reviewers made specific and valuable recommendations and corrections that improved the quality of my publication. I strongly recommend this Journal.

Dr. Katarzyna Byczkowska My testimonial covering: "The peer review process is quick and effective. The support from the editorial office is very professional and friendly. Quality of the Clinical Cardiology and Cardiovascular Interventions is scientific and publishes ground-breaking research on cardiology that is useful for other professionals in the field.
Thank you most sincerely, with regard to the support you have given in relation to the reviewing process and the processing of my article entitled "Large Cell Neuroendocrine Carcinoma of The Prostate Gland: A Review and Update" for publication in your esteemed Journal, Journal of Cancer Research and Cellular Therapeutics". The editorial team has been very supportive.

Testimony of Journal of Clinical Otorhinolaryngology: work with your Reviews has been a educational and constructive experience. The editorial office were very helpful and supportive. It was a pleasure to contribute to your Journal.

Dr. Bernard Terkimbi Utoo, I am happy to publish my scientific work in Journal of Women Health Care and Issues (JWHCI). The manuscript submission was seamless and peer review process was top notch. I was amazed that 4 reviewers worked on the manuscript which made it a highly technical, standard and excellent quality paper. I appreciate the format and consideration for the APC as well as the speed of publication. It is my pleasure to continue with this scientific relationship with the esteem JWHCI.

This is an acknowledgment for peer reviewers, editorial board of Journal of Clinical Research and Reports. They show a lot of consideration for us as publishers for our research article “Evaluation of the different factors associated with side effects of COVID-19 vaccination on medical students, Mutah university, Al-Karak, Jordan”, in a very professional and easy way. This journal is one of outstanding medical journal.
Dear Hao Jiang, to Journal of Nutrition and Food Processing We greatly appreciate the efficient, professional and rapid processing of our paper by your team. If there is anything else we should do, please do not hesitate to let us know. On behalf of my co-authors, we would like to express our great appreciation to editor and reviewers.

As an author who has recently published in the journal "Brain and Neurological Disorders". I am delighted to provide a testimonial on the peer review process, editorial office support, and the overall quality of the journal. The peer review process at Brain and Neurological Disorders is rigorous and meticulous, ensuring that only high-quality, evidence-based research is published. The reviewers are experts in their fields, and their comments and suggestions were constructive and helped improve the quality of my manuscript. The review process was timely and efficient, with clear communication from the editorial office at each stage. The support from the editorial office was exceptional throughout the entire process. The editorial staff was responsive, professional, and always willing to help. They provided valuable guidance on formatting, structure, and ethical considerations, making the submission process seamless. Moreover, they kept me informed about the status of my manuscript and provided timely updates, which made the process less stressful. The journal Brain and Neurological Disorders is of the highest quality, with a strong focus on publishing cutting-edge research in the field of neurology. The articles published in this journal are well-researched, rigorously peer-reviewed, and written by experts in the field. The journal maintains high standards, ensuring that readers are provided with the most up-to-date and reliable information on brain and neurological disorders. In conclusion, I had a wonderful experience publishing in Brain and Neurological Disorders. The peer review process was thorough, the editorial office provided exceptional support, and the journal's quality is second to none. I would highly recommend this journal to any researcher working in the field of neurology and brain disorders.

Dear Agrippa Hilda, Journal of Neuroscience and Neurological Surgery, Editorial Coordinator, I trust this message finds you well. I want to extend my appreciation for considering my article for publication in your esteemed journal. I am pleased to provide a testimonial regarding the peer review process and the support received from your editorial office. The peer review process for my paper was carried out in a highly professional and thorough manner. The feedback and comments provided by the authors were constructive and very useful in improving the quality of the manuscript. This rigorous assessment process undoubtedly contributes to the high standards maintained by your journal.

International Journal of Clinical Case Reports and Reviews. I strongly recommend to consider submitting your work to this high-quality journal. The support and availability of the Editorial staff is outstanding and the review process was both efficient and rigorous.

Thank you very much for publishing my Research Article titled “Comparing Treatment Outcome Of Allergic Rhinitis Patients After Using Fluticasone Nasal Spray And Nasal Douching" in the Journal of Clinical Otorhinolaryngology. As Medical Professionals we are immensely benefited from study of various informative Articles and Papers published in this high quality Journal. I look forward to enriching my knowledge by regular study of the Journal and contribute my future work in the field of ENT through the Journal for use by the medical fraternity. The support from the Editorial office was excellent and very prompt. I also welcome the comments received from the readers of my Research Article.

Dear Erica Kelsey, Editorial Coordinator of Cancer Research and Cellular Therapeutics Our team is very satisfied with the processing of our paper by your journal. That was fast, efficient, rigorous, but without unnecessary complications. We appreciated the very short time between the submission of the paper and its publication on line on your site.

I am very glad to say that the peer review process is very successful and fast and support from the Editorial Office. Therefore, I would like to continue our scientific relationship for a long time. And I especially thank you for your kindly attention towards my article. Have a good day!
"We recently published an article entitled “Influence of beta-Cyclodextrins upon the Degradation of Carbofuran Derivatives under Alkaline Conditions" in the Journal of “Pesticides and Biofertilizers” to show that the cyclodextrins protect the carbamates increasing their half-life time in the presence of basic conditions This will be very helpful to understand carbofuran behaviour in the analytical, agro-environmental and food areas. We greatly appreciated the interaction with the editor and the editorial team; we were particularly well accompanied during the course of the revision process, since all various steps towards publication were short and without delay".

I would like to express my gratitude towards you process of article review and submission. I found this to be very fair and expedient. Your follow up has been excellent. I have many publications in national and international journal and your process has been one of the best so far. Keep up the great work.

We are grateful for this opportunity to provide a glowing recommendation to the Journal of Psychiatry and Psychotherapy. We found that the editorial team were very supportive, helpful, kept us abreast of timelines and over all very professional in nature. The peer review process was rigorous, efficient and constructive that really enhanced our article submission. The experience with this journal remains one of our best ever and we look forward to providing future submissions in the near future.

I am very pleased to serve as EBM of the journal, I hope many years of my experience in stem cells can help the journal from one way or another. As we know, stem cells hold great potential for regenerative medicine, which are mostly used to promote the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. I think Stem Cell Research and Therapeutics International is a great platform to publish and share the understanding towards the biology and translational or clinical application of stem cells.

I would like to give my testimony in the support I have got by the peer review process and to support the editorial office where they were of asset to support young author like me to be encouraged to publish their work in your respected journal and globalize and share knowledge across the globe. I really give my great gratitude to your journal and the peer review including the editorial office.

I am delighted to publish our manuscript entitled "A Perspective on Cocaine Induced Stroke - Its Mechanisms and Management" in the Journal of Neuroscience and Neurological Surgery. The peer review process, support from the editorial office, and quality of the journal are excellent. The manuscripts published are of high quality and of excellent scientific value. I recommend this journal very much to colleagues.

Dr.Tania Muñoz, My experience as researcher and author of a review article in The Journal Clinical Cardiology and Interventions has been very enriching and stimulating. The editorial team is excellent, performs its work with absolute responsibility and delivery. They are proactive, dynamic and receptive to all proposals. Supporting at all times the vast universe of authors who choose them as an option for publication. The team of review specialists, members of the editorial board, are brilliant professionals, with remarkable performance in medical research and scientific methodology. Together they form a frontline team that consolidates the JCCI as a magnificent option for the publication and review of high-level medical articles and broad collective interest. I am honored to be able to share my review article and open to receive all your comments.

“The peer review process of JPMHC is quick and effective. Authors are benefited by good and professional reviewers with huge experience in the field of psychology and mental health. The support from the editorial office is very professional. People to contact to are friendly and happy to help and assist any query authors might have. Quality of the Journal is scientific and publishes ground-breaking research on mental health that is useful for other professionals in the field”.
Dear editorial department: On behalf of our team, I hereby certify the reliability and superiority of the International Journal of Clinical Case Reports and Reviews in the peer review process, editorial support, and journal quality. Firstly, the peer review process of the International Journal of Clinical Case Reports and Reviews is rigorous, fair, transparent, fast, and of high quality. The editorial department invites experts from relevant fields as anonymous reviewers to review all submitted manuscripts. These experts have rich academic backgrounds and experience, and can accurately evaluate the academic quality, originality, and suitability of manuscripts. The editorial department is committed to ensuring the rigor of the peer review process, while also making every effort to ensure a fast review cycle to meet the needs of authors and the academic community. Secondly, the editorial team of the International Journal of Clinical Case Reports and Reviews is composed of a group of senior scholars and professionals with rich experience and professional knowledge in related fields. The editorial department is committed to assisting authors in improving their manuscripts, ensuring their academic accuracy, clarity, and completeness. Editors actively collaborate with authors, providing useful suggestions and feedback to promote the improvement and development of the manuscript. We believe that the support of the editorial department is one of the key factors in ensuring the quality of the journal. Finally, the International Journal of Clinical Case Reports and Reviews is renowned for its high- quality articles and strict academic standards. The editorial department is committed to publishing innovative and academically valuable research results to promote the development and progress of related fields. The International Journal of Clinical Case Reports and Reviews is reasonably priced and ensures excellent service and quality ratio, allowing authors to obtain high-level academic publishing opportunities in an affordable manner. I hereby solemnly declare that the International Journal of Clinical Case Reports and Reviews has a high level of credibility and superiority in terms of peer review process, editorial support, reasonable fees, and journal quality. Sincerely, Rui Tao.
Clinical Cardiology and Cardiovascular Interventions I testity the covering of the peer review process, support from the editorial office, and quality of the journal.
